JAMA: Among women with metastatic breast cancer, treatment with a drug that
is biosimilar to the breast cancer drug trastuzumab resulted in an
equivalent overall response rate at 24 weeks compared with trastuzumab,
according to a study published online by JAMA. Biological agents, including monoclonal antibodies, have increased
the treatment options and greatly improved outcomes for a number of
cancers. However, patient access to these biologics is limited in many
countries. With impending patent expiration of some biological agents,
development of biosimilars has become a high priority for drug
developers and health authorities throughout the world to provide access
to high-quality alternatives. A biosimilar drug is a biological product
that is highly similar to a licensed biological product, with no
clinically meaningful differences in terms of safety or potency.
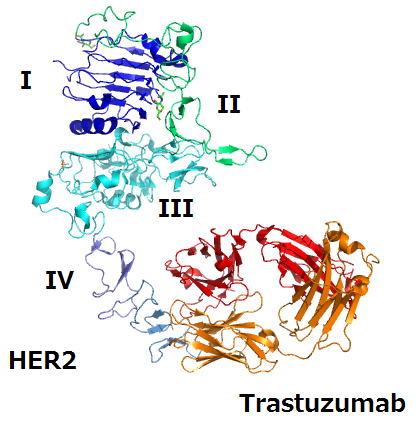
Treatment with the anti-ERBB2 humanized monoclonal antibody
trastuzumab and chemotherapy significantly improves progression-free and
overall survival in patients with ERBB2 (HER2)-positive metastatic
breast cancer. In this multicenter, phase 3 study, Hope S. Rugo, M.D.,
of the University of California San Francisco Helen Diller Family
Comprehensive Cancer Center, and colleagues randomly assigned patients
with ERBB2-positive metastatic breast cancer to receive a proposed
trastuzumab biosimilar (MYL-14010) (n = 230) or trastuzumab (n = 228)
with a taxane (a chemotherapy agent) to compare the overall response
rate and safety after 24 weeks. Chemotherapy was administered for at
least 24 weeks followed by antibody alone until unacceptable toxic
effects or disease progression occurred. Tumor was assessed every 6
weeks. The primary outcome was week 24 overall response rate defined as
complete or partial response.
The overall response rate was 70 percent for the proposed biosimilar
vs 64 percent for trastuzumab. At week 48, there was no statistically
significant difference with the proposed biosimilar vs trastuzumab for
time to tumor progression (41 percent vs 43 percent), progression-free
survival (44 percent vs 45 percent), or overall survival (89 percent vs
85 percent). In the proposed biosimilar and trastuzumab groups, 99
percent and 95 percent of patients had at least 1 adverse event.
“Trastuzumab is not widely available around the world,” the authors
write. “A biosimilar treatment option may increase global access to
biologic cancer therapies, provided, among other issues, that the price
of the biosimilar is sufficiently inexpensive to enable women in
non-high-income countries to access this therapy.”
The researchers note that further study is needed to assess safety as well as long-term clinical outcome.
(doi:10.1001/jama.2016.18305; the study is available pre-embargo at the For the Media website)