Authors: Drs Marshall Stoller (university of California SF) and Aaron Berger (Chicago) 2009-12-10
Introduction:
The
kidneys are paired organs with the primary function of helping to remove
toxins from the body and regulate water balance; they are vital to
survival. After urine is produced in the kidneys, it must
pass down to the bladder where it can be stored before being eliminated
from the body through the urethra. At almost any point in this pathway, urine can become obstructed and may lead to kidney damage. When severe, this can cause a patient to require a kidney transplant or dialysis to sustain life. Obstruction can be present from birth or it may develop later in life. The most common causes of obstruction include stones, strictures, tumors, and bladder dysfunction. This article will discuss the various causes and treatments of urinary tract obstruction.
Relevant Anatomy:
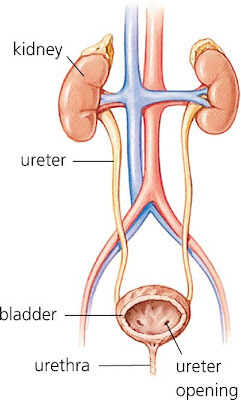
The
urinary tract has several main components including the kidneys which
form the urine, the ureters which transport the urine to the bladder,
which then stores the urine until it passes out of the body through the
urethra.
The kidneys are paired, bean shaped organs located in the back just below the ribs. They
serve multiple functions in the body, but primarily the kidneys filter
the blood to clear toxins and extra water from the body by producing
urine. Blood is filtered by a specialized structure called the glomerulus. Filtered
blood from the glomeruli passes into a complex and highly specialized
tubular system that runs through the kidney called the nephron that
adjusts the concentration of the urine, and is responsible for the
excretion or absorption of the various electrolytes such as sodium and
potassium. There are three main parts of the kidney .
The
cortex is the outer portion of the kidney where all the specialized
filters (glomeruli) and tubular structures (nephrons) that filter the
blood and concentrate the urine are located. The medulla is where the final concentration of the urine is adjusted prior to entering the collecting system. The
collecting system is where the urine empties before passing down the
ureters, which are the long thin tubes (about 2-4mm in diameter and
25-30cm in length) that channel the urine into the bladder. The
collecting system is comprised of a branch network of structures called
calyces which all empty into the renal pelvis, which then funnels the
urine into the ureters. The ureters empty into the bladder where the urine is stored until the urine is eliminated from the body through the urethra. Obstruction
may occur along almost any point in this pathway and can lead to
symptoms such as pain, nausea, vomiting, fevers, chills and,
potentially, damage to the kidneys.
Signs, Symptoms, Diagnosis:
The hallmark of urinary tract obstruction is dilation of the collecting system of the kidney which is known as hydronephrosis. This swelling typically causes pain in the flank or upper abdomen on the affected side. Sometimes, the pain may be severe enough to cause nausea or even vomiting.
When hydronephrosis is present, the kidney is not draining urine normally so there can be stasis (slowing or stopping of the flow) of urine in the collecting system. This may lead to urinary tract infection or stone formation so patients may present with signs of infection such as fevers, chills, or pain or burning with urination (dysuria).
The evaluation of urinary
tract obstruction often includes a urinalysis to look for: signs of
infection, blood in the urine, a white blood cell count which if
elevated can signify infection, and a serum creatinine level which is an
approximate measure of total kidney function and is often elevated in
cases of obstruction. There are multiple imaging modalities that can be used in the diagnosis of urinary tract obstruction. Ultrasound
is readily available, causes no radiation exposure, and can easily
identify hydronephrosis, but may not always be able to identify the
cause. Ultrasound may be used to determine if the bladder is distended and a possible source of hydronephrosis. An
intravenous urogram (IVU) is a study where the patient is given a
contrast dye injection and then plain x-rays are taken at several points
in time. This study used to be very commonplace and
provides useful information, but has been replaced for the most part by
computed tomography (CT). CT scans can be performed with
and without intravenous contrast and can provide useful information not
only about the urinary tract, but other intra-abdominal organs as well,
which can enable the practitioner to look for other types of pathology
which may be causing obstruction. Magnetic resonance
imaging is also a useful modality in the evaluation of urinary tract
obstruction, but it has the disadvantage of being more costly, less
readily available, more time consuming, and it does not detect kidney
stones very well. In many cases of urinary tract obstruction, a nuclear renal scan is obtained. During
this exam, a radiotracer (a radioactive solution) is given
intravenously and then scans are performed at multiple time points. The
figure below shows a normal kidney on the right and an obstructed
kidney on the left as the tracer concentrates slowly and does not drain
from the kidney.
These
studies provide useful information about the function of the kidneys in
relation to one another and help clarify how severe the obstruction is.
Urinary Stone Disease:
Stones
may occur in any part of the urinary tract and affect roughly 10% of
the population. (A detailed discussion of stone disease and treatment
can be found in the kidney stone Knol ) Stones typically
cause obstruction as they pass from the kidney, down the ureter toward
the bladder, but larger stones may obstruct a portion of the kidney or
the entire kidney if they are located in the renal pelvis. The
three most common locations for stones to cause obstruction are at the
point where the renal pelvis joins with the ureter (ureteropelvic
junction), the point where the ureters pass over the iliac artery and
vein in the pelvis, and where the ureter joins the bladder
(ureterovesical junction). There are multiple types of
stones but the majority of stones, with the exception of uric acid
stones, cannot be dissolved with medications and must either pass out of
the body on their own or be removed with a urologic intervention. Small
stones (less than 5mm) have a strong likelihood of passing into the
bladder and subsequently out of the urethra, but the chances decrease
dramatically with larger stones. Stone passage can be
aided by several medications including alpha-blockers (tamsulosin
(Flomax), alfuzosin (Uroxatral), terazosin (Hytrin), doxazosin
(Cardura)), steroids (prednisone, methylprednisolone), and non-steroidal
anti-inflammatory medications (ibuprofen, naproxen). All of these help
decrease inflammation and relax the smooth muscle in the ureter to help
stones pass. If medical expulsion therapy fails, there are multiple surgical options for treatment of stones. If
the patients are very sick, a drainage procedure to relieve the
obstruction is performed and this can either be with a ureteral stent or
a nephrostomy tube. A stent is a small plastic straw-like tube placed into the ureter to allow urine to drain past an obstructing stone.
A
nephrostomy tube is a small drainage tube placed directly into the
kidney through the skin of the back which allows the kidney to drain. For
definitive management of the stones, the options include shock wave
lithotripsy (SWL), ureteroscopy, percutaneous nephrolithotomy (PNL), or
open surgical removal.
Shock wave
lithotripsy is a non-invasive procedure during which a patient lies on a
special table and shock waves are targeted at the stone with a goal of
fragmenting the stone into tiny pieces which may subsequently pass.
Ureteroscopy
is a minimally invasive procedure during which a small scope is placed
into the bladder, the opening to the ureter is identified, and then a
smaller scope (ureteroscope) is placed into the ureter. The stone is then visualized and broken up with a laser or with other means and removed with a basket or graspers.
During
a percutaneous nephrolithotomy, a tract is formed directly into the
kidney from the back and stones are broken up and suctioned out using a
variety of devices. This procedure requires a small incision in the back and is often reserved for larger and/or more complex stones.
In
most cases, after the obstructing stone has passed or has been removed,
the kidney function returns to normal but in some cases of longstanding
obstruction, permanent loss of kidney function can occur. It is unclear how long a kidney may remain obstructed and still retain viable function.
Ureteropelvic Junction Obstruction (UPJO):
The
ureteropelvic junction is where the renal pelvis joins with the ureter
as urine is funneled out of the kidney into the ureter.
Obstruction
of the UPJ can be congenital or acquired. It can cause significant
obstruction of the affected kidney and may lead to loss of kidney
function over time.
The congenital
causes of UPJO are thought to be due to either a weak segment of ureter,
a section with abnormal muscle development so urine is not propelled
downwards, or a crossing blood vessel or tissue band which can cause
obstruction. It is unusual for children presenting with
UPJ obstruction to have a crossing vessel, although they are present in
about half of patients who present as adults. Acquired causes can be due to kidney stones or prior surgical interventions which can cause subsequent scarring.
UPJ obstructions may be asymptomatic or they may present with pain, nausea, vomiting, or urinary tract infections. Patients
with symptomatic UPJO often complain of worsening pain after drinking
large amounts of fluid, especially alcohol which is a diuretic and
causes the kidney to fill with urine more quickly thereby worsening the
distention. The age at presentation of UPJO is highly
variable with some cases being diagnosed on prenatal ultrasonography and
others not presenting until late in life; it is unclear exactly what
triggers the onset of symptoms.
Imaging
of the affected kidney with ultrasound or computed tomography (CT)
scanning demonstrates swelling of the collecting system
(hydronephrosis). A nuclear renal scan is often utilized
to assess not only the function of the obstructed kidney, but also the
degree of obstruction. During this test, radiotracer is injected intravenously (in the vein) and then several scans are performed over time. A
normal kidney will take up the radiotracer quickly and then excrete it
into the urine and down into the bladder in a matter of several minutes. In
a kidney with an UPJO, the uptake of tracer can be decreased if there
is functional damage to the kidney and there is often poor drainage of
the tracer from the kidney, which is indicative of obstruction.
There are several treatment options for a UPJO. For
symptomatic patients awaiting definitive repair or patients unable to
undergo more extensive surgery, a ureteral stent or a nephrostomy tube
can relieve the obstruction.
Another
more definitive treatment option is an endopyelotomy which can be
performed either in a retrograde fashion (from the bladder up towards
the kidney) with an ureteroscope or in an antegrade fashion via a
percutaneous approach similar to that discussed earlier for the
treatment of stones. During an endopyelotomy, a full
thickness incision is made in the lateral aspect of the diseased UPJ
with a knife, laser, or electrocautery device. A stent is
then typically left in place for 2-6 weeks to allow for healing and is
subsequently removed. These procedures have a long term success rate of
approximately 70-75% meaning that post-operatively, the UPJ drains well
and patients have symptomatic and radiographic improvement. The success of endopyelotomy decreases in cases with a crossing vessel.
Another
treatment option is a pyeloplasty which can either be performed open,
typically with an incision through the flank, or laparoscopically using
only three or four small (about 1cm) incisions in the abdomen. During
the most common form of pyeloplasty, the diseased segment of the UPJ is
completely excised and the ureter is then reattached to the renal
pelvis.
If
there is a crossing vessel, the ureter/renal pelvis is transposed above
(anterior) to the vessel to avoid recurrent obstruction. The
success rate for either open or laparoscopic pyeloplasty is better than
90% in most published reports and appears to be durable over the long
term. A successful outcome is usually based on symptomatic improvement for the patient but may also include radiographic improvement. A ureteral stent is typically left in place for several weeks after a pyeloplasty to allow the reconstructed UPJ to heal. If
the kidney no longer has much function due to long standing
obstruction, the best option may be to just remove the kidney,
especially if the patient has a history of recurrent urinary tract
infections and/or pain. Again, the kidney may be removed
either with a traditional open approach or may be done laparoscopically
which offers more rapid recovery with improved cosmetic results (see
Laparoscopic Renal Surgery Knol).
Ureteral Strictures
Strictures may occur anywhere in the ureter and are often the result of stones or prior surgery leading to scar tissue. Some infections diseases, however, such as tuberculosis may also cause scarring of the ureter. Strictures
may occur at the distal portion of the ureter, especially in cases
where ureteral reconstruction has occurred such as in kidney transplants
where the donated ureter is attached to the bladder. Another example of this is in patients with invasive bladder cancer where the bladder has been surgically removed. In
these cases, the ureters are usually connected to an isolated segment
of bowel which is used to create a new bladder or a conduit to the skin
for the urine to drain, and these are known as ureteroenteric
anastomotic strictures.
Similar to a
UPJ obstruction, ureteral strictures or ureteroenteric anastomotic
strictures can often be managed with a minimally invasive approach
either via an ureteroscopic or percutaneous approach. The
strictures can be incised with a laser, an endoscopic knife, an
electrocautery probe, or they may be dilated with a ureteral balloon
dilator. These techniques work well for short strictures
(less than 1cm) but for longer strictures, more extensive procedures are
required for long term success.
For
longer strictures in the distal ureter, a ureteral reimplantation can be
performed and may be combined with a procedure called a psoas
hitch/Boari flap. In these procedures, the ureter is disconnected from the bladder and the diseased segment is excised. The
bladder is then freed up from some of its attachments; this often
provides enough length to reach the more proximal healthy ureter and the
ureter is sewn back into the bladder. If the distance is
too far to bridge, a bladder flap is created and rotated up toward the
ureter and then sewn into a tube which is called a Boari flap. During this procedure, the bladder is fixed to the psoas muscle tendon to reduce tension on the repair (psoas hitch). Some
strictures in the mid or proximal ureter may be repaired by simply
excising the narrowed segment and sewing the two ends of the ureter back
together, a procedure known as a ureteroureterostomy For long
strictures in the proximal portion of the ureter, the ureter may be
replaced by a segment of intestine (ileal interposition) or the kidney
may be removed and then transplanted into the patient’s pelvis near the
bladder (auto-transplantation).
Obstruction from Malignancy:
The ureters may be affected by cancers occurring both inside and outside the urinary system. Almost
the entire urinary tract is lined by cells known as transitional cells
and these may develop cancers known as transitional cell carcinomas
(TCC) or urothelial carcinoma. TCC most commonly occurs in the bladder but may also occur in the ureter or in the collecting system of the kidney. Tumors of the ureter and larger tumors in the renal pelvis may lead to obstruction of the kidney.
The
recommended treatment for cancer in the ureter or collecting system of
the kidney is a nephroureterectomy where the kidney and the entire
ureter are removed all the way down to the bladder. The
reason for this is that urothelial carcinoma is thought to be a defect
of the entire lining of the kidney, ureter, and bladder known as a field
change defect and a tumor in the ureter has a high likelihood of
recurring in the kidney and the bladder. This procedure may be performed in either an open or laparoscopic fashion.
For
patients who cannot tolerate this relatively large operation or those
with a solitary kidney or other risk factors for poorly functioning
kidneys such as high blood pressure or diabetes mellitus, a minimally
invasive approach can be utilized. Tumors in the ureter or
collecting system of the kidney can be resected or fulgurated
(destroyed by electric current) with either cautery or laser via an
ureteroscopic or percutaneous approach. Patients treated with these techniques require frequent surveillance as these tumors often recur. Occasionally, large tumors in the bladder may cause obstruction of one or both ureteral orifices and lead to kidney obstruction. In these cases, resection of the bladder tumor is necessary to relieve the blockage.
There are a variety of malignancies which may cause obstruction of the urinary tract by compressing the ureter from the outside. In
these cases, the best and often only way to treat the obstruction is to
try to reduce the size of the cancer either surgically or with
chemotherapy or radiation.
Retroperitoneal Fibrosis (RPF):
The
kidneys and ureters are located in what is known as the
retroperitoneum, which means behind the peritoneal sac which contains
the majority of the intestines. Retroperitoneal fibrosis
is a disease where a fibrous process envelops either one but typically
both ureters which causes compression and subsequent kidney obstruction. Several
medications are known to cause RPF but most commonly, the process is
idiopathic meaning that no definitive cause can be identified.
Patients
with RPF can sometimes be managed with ureteral stents to relieve the
obstruction, but in many cases, the fibrotic process is strong enough to
compress stents and the obstruction recurs. In these cases, a nephrostomy tube can be placed or the patient can undergo a procedure called ureterolysis. During
an ureterolysis, which can be performed either open or
laparoscopically, the ureter is released from the fibrotic process and
then either placed inside the peritoneal cavity or wrapped with a
protective layer or fat called omentum, to help prevent the fibrotic
process from recurring. During this procedure, a biopsy of the fibrous tissue is made to confirm the diagnosis and exclude cancer.
Congenital Ureteral Anomalies:
In
addition to ureteropelvic junction obstruction, there are several other
causes of ureteral obstruction that may be due to congenital
abnormalities. In some patients, the ureter inserts into an abnormal location (ectopic) in the bladder which may lead to obstruction. This
condition is more common in patients with a duplicated collecting
system where there are two ureters and two collecting systems
originating in the same kidney, and one of the ureters often is ectopic
and leads to obstruction.
This
condition may be treated by reimplanting the obstructed ureter into
another location in the bladder or by attaching the obstructed ureter
into the non-obstructed ureter from the same kidney
(uretero-ureterostomy). If there is long-standing
obstruction, the portion of the kidney drained by the obstructed ureter
may lose function and the best treatment may be to remove this portion
of the kidney along with its obstructed ureter, leaving the remaining
viable portion of the kidney intact.
A typical ureter lies above the large vein running above the spine called the inferior vena cava (IVC). However,
some patients have what is known as a retrocaval or circumcaval ureter
where the ureter courses behind this large vein and may lead to
obstruction. This is managed by dividing the ureter and then re-connecting it in front of (anterior) the IVC.
Another congenital condition that may cause urinary tract obstruction is an ureterocele. This
is a cystic outpouching of the ureter as it enters the bladder and
forms a small balloon like sac in the bladder which may obstruct the
flow of urine from the affected kidney, and if large enough, may even
obstruct the flow of urine from the opposite kidney. The
ureterocele can be punctured endoscopically (through a tube) or, in
larger cases, may be excised and the ureter reimplanted into a different
location in the bladder.
Neurogenic Bladder:
A normal bladder stores urine at low pressures until it gets close to its capacity, often around 400cc. In
many patients with neurologic diseases such as a spinal cord injury,
the bladder has decreased compliance meaning that the pressure in the
bladder increases significantly as it fills with urine (bladder becomes
stiff). This high pressure can cause the urine flowing
down the ureters from the kidneys to get backed up resulting in
obstruction and hydronephrosis (swelling of the kidneys) in the kidneys. Over time, this can lead to deterioration of renal function.
The
treatment of this process is aimed at decreasing the pressure in the
bladder which can be accomplished with various medications, as well as
keeping the bladder relatively empty by having the patients urinate
frequently. In many cases, patients are unable to urinate
normally so a catheter can be left in the bladder, or a catheter may be
placed into the bladder to empty the urine several times daily; this is
referred to as clean intermittent catheterization (CIC). The
goal of CIC in most patients with a neurogenic bladder should be to
catheterize as frequently as necessary to keep the total volume to 400cc
or less as this will prevent infections and preserve renal function. In
some severe cases, when these more conservative methods fail, the urine
must be diverted by creating a low pressure urinary diversion with a
loop of intestine draining into a bag on the skin which is known as an
ileal conduit. With proper bladder drainage and medications, many patients with neurogenic bladders are able to preserve their renal function.
Obstruction from Benign Prostatic Hyperplasia (BPH):
As
men get older, the prostate typically becomes larger and may cause
bothersome urinary symptoms such as frequency, urgency, and incomplete
bladder emptying. In some cases, the prostate may become
so obstructive that the bladder is always full and urine only leaks out
in small amounts when the bladder capacity is exceeded, a condition
known as overflow incontinence. When this occurs, the
urine does not drain normally from the kidneys as there is nowhere for
it to drain so hydronephrosis may occur. If left untreated, this may
lead to deterioration of renal function.
The
initial treatment for urinary obstruction due to prostatic enlargement
is to place a catheter into the bladder to allow the urinary system to
decompress. Once this is accomplished, there are multiple
options for managing BPH and these are discussed in detail in the benign
prostatic hyperplasia Knol.
Urethral Stricture Disease:
The urethra is the tube where the urine passes on its way out of the body from the bladder. Narrowing
or stricturing of the urethra may occur as a result of a congenital
defect, infection (typically gonorrhea or chlamydia), or trauma such as a
straddle injury (e.g., falling onto the crossbar of a bicycle). In
rare cases, if the stricture is severe, the urine may not be able to
pass through the urethra and the bladder becomes chronically filled,
which may subsequently lead to hydronephrosis.
Urethral
strictures may be treated by dilation, incision with a small endoscopic
knife (direct visual internal urethrotomy), or with a larger
reconstructive operation known as an urethroplasty where the narrowed
segment is excised and the two healthy ends of the urethra are
re-attached. In some cases of long urethral strictures,
some type of tissue flap may be needed to help bridge the gap to allow
for reconstruction. In addition to strictures of the more
proximal urethra, sometimes there is obstruction at the end of the
urethra which is known as urethra meatal stenosis. This
can be corrected either by dilating the urethral opening or
occasionally, the natural opening may need to be widened surgically to
allow better urine flow. In men, the foreskin can also
become obstructive, either from congenital tightness or scarring from
infection, a condition known as phimosis. Typically, a circumcision is necessary to treat a phimosis severe enough to cause difficulty passing the urine.
Posterior Urethral Valves:
Posterior
urethral valves (PUV) are a congenital anatomic defect of the male
urethra that may lead to severe urethral obstruction in infants and
cause bladder distention, and hydronephrosis. The valves are small flaps of tissue that in normal males regress into non-obstructing urethral folds. PUV
are often diagnosed on prenatal ultrasonography by a markedly dilated
bladder, elongated posterior urethra, and hydronephrosis in both
kidneys.
The obstruction is initially
relieved by placement of a catheter into the bladder and the valves can
subsequently be incised endoscopically. In some cases,
the bladder is sewn directly to a small opening in the skin
(vesicostomy) to allow for drainage until the child undergoes a
definitive valve ablation. As this is a congenital
condition, even prompt intervention post-natally may be unable to
reverse any pre-existing damage to the kidneys.
Conclusions:
There are many different types of urinary tract obstructions. These
obstructions may result in swelling (hydronephrosis) of one or both
kidneys, which if left untreated may lead to deterioration of renal
function. The treatment of the obstruction may range from
simple observation – as in the case of a small kidney stone – or may
require major reconstructive surgery. It is important to have a discussion with your urologist regarding the risks and benefits of all the treatment options. The
bottom line is that all efforts should be made to preserve kidney
function to avoid the need for dialysis or renal transplantation.