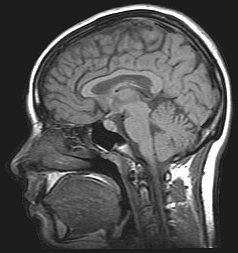
Oregon: Neuroimaging of the brain using technologies such as magnetic
resonance imaging, or MRIs, increasingly is showing promise as a
technique to predict adolescent vulnerability to substance abuse
disorders, researchers conclude in a new analysis. A greater understanding of what such technologies offer
and continued research to perfect the use of them may ultimately help
identify youth at the highest risk for these problems and allow
prevention approaches. These might include neuropsychological
intervention exercises that can strengthen vulnerable cognitive networks
in the brain.
The findings are of importance, researchers say, because underage
alcohol and drug use is increasingly being recognized as a public health
and social problem, with long-term consequences that include poorer
academic performance, neurocognitive deficits and psychosocial problems.
Youth who begin drinking before age 15 have four to six times the
rate of lifetime alcohol dependence than those who do not drink by age
21, researchers noted in this analysis, which was recently published in
Current Opinion in Behavioral Sciences.
“Structural and neural alterations in the brain from drug and alcohol
abuse have now been well established,” said Anita Cservenka, an
assistant professor in the College of Liberal Arts at Oregon State
University, and co-author of the study.
“It’s also becoming clear that some of these alterations can exist
before any substance abuse, and often are found in youth who have a
family history of alcohol and drug use disorders. These familial risk
factors can play a role in future substance abuse, along with
environmental risk factors such as peer influence, personality and
psychosocial interactions.”
Family history of alcohol-use disorder is a strong predictor of
substance abuse, Cservenka said, as it raises the risk for the
development of alcohol-use disorder in adolescents by three to five
times. Neuroimaging studies show significant overlap in brain scans
between those with a family history of alcohol- and substance-use
disorders and youth who begin using substances during adolescence.
Some of the findings in youth with family history of alcohol- and
substance-use disorder include a smaller volume of limbic brain regions,
sex-specific patterns of hippocampal volume, and a positive association
of familial risk with “nucleus accumbens” volume in the brain. Other
risk factors for adolescent substance use that have been identified
include poorer performance on executive functioning tasks of inhibition
and working memory, smaller brain volumes in reward and cognitive
control regions, and heightened response to rewards.
A factor contributing to a peak in substance use during adolescence,
researchers say, may be emotion and reward systems that develop before
cognitive control systems, leaving youth more vulnerable to risk-taking
behaviors.
Almost two thirds of 18-year-olds, for instance, support lifetime
alcohol use; 45 percent marijuana use; and 31 percent smoking
cigarettes.
Various studies, Cservenka said, are examining such issues, including
the National Consortium on Alcohol and Neurodevelopment in Adolescence,
which includes five sites across the U.S. following 800 youth ages
12-21.
“We’re just beginning to understand the risk factors for substance
abuse and the consequences of adolescent substance use with these types
of large, long-term studies,” she said. “Ultimately such information
should help inform us about who might be at most risk and what brain
areas are most vulnerable, so we can target them and work to prevent the
problems.”
If an MRI showed weakness in working memory, for instance, computer
games or behavioral tasks might help strengthen the area of the brain
that is deficient. Similar approaches might also be used to help address
issues such as stress and depression, Cservenka said.
The lead author on this review was Lindsay Squeglia at the Medical
University of South Carolina. The work has been supported by the
National Institutes of Health.