UCSD: Accurately assessing pain in children in a clinical setting can be
difficult. A study by researchers at the University of California, San
Diego School of Medicine has demonstrated the validity of a new method
for measuring pediatric pain levels using novel facial pattern
recognition software. The study is published in the journal Pediatrics.
“The current methods by which we analyze pain in kids are
suboptimal,” said senior author Jeannie Huang, MD, MPH, a professor in
the UC San Diego School of Medicine Department of Pediatrics and a
gastroenterologist at Rady Children’s Hospital-San Diego. “In this
study, we developed and tested a new instrument, which allowed us to
automatically assess pain in children in a clinical setting. We believe
this technology, which enables continuous pain monitoring, can lead to
better and more timely pain management.”
The researchers used the software to analyze pain-related facial
expressions from video taken of 50 youths, ages five to 18 years old,
who had undergone laparoscopic appendectomies at Rady Children’s
Hospital-San Diego. Based on the analysis, along with clinical data
input by the study team, the software provided pain level scores for
each participant.
Huang said controlling pain is important, not only for the child’s
comfort, but also for recovery. Studies have shown that under-treatment
of pain is associated with adverse surgical outcomes. “Accurate
assessment of pain is a fundamental tenet of delivery of care,” she
said.
Several issues, particularly age-related communication difficulties,
make existing pediatric pain assessment methods problematic, said Huang.
“The current gold standard for measuring pain is self-reporting,” she
said, noting patients are generally asked to rate their pain on a scale
of zero to 10. “But in pediatrics there is a limited population of kids
who can answer that question in a meaningful way. Younger children can
have difficulty - a two-year-old hasn’t developed the cognitive and
conceptual abilities to think in those terms.”
Clinical pain assessments, aided by nurses or parents, are often used
in lieu of patient self-report in children because of these
limitations. However, several previous studies have shown nursing staff
may have difficulty accurately estimating pain (often underestimating
pain), particularly among pediatric patients. Parents are generally more
in tune with their children’s pain levels, but may not always be
available, said Huang.
Another problem with pain assessment protocols, Huang added, is that
pain checks tend to be scheduled and consequently may not coincide with
times when pain occurs and when intervention is needed. “Pain
assessments are typically scheduled along with vital signs, the
frequency of which can vary from every 4 to 8 hours depending on patient
severity.”
In the study, researchers filmed the participants at three different
visits post-surgery: within 24 hours after an appendectomy; one calendar
day after the first visit and at a follow-up visit 2 to 4 weeks after
surgery. Facial video recordings and self-reported pain ratings by the
participant and pain ratings by parents and nurses were collected.
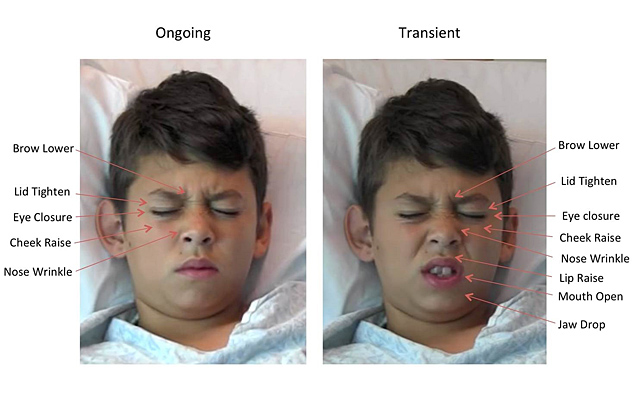
The research team sought to determine the software’s accuracy at pain
measurement as compared to self-reporting by the child and as compared
to by proxy estimations by parents and nurses. The software prototype
utilized data collected via prior software (Computer Expression
Recognition Toolbox) by study co-author Marian Bartlett, PhD, at UC San
Diego’s Institute for Neural Computation, which utilizes computer vision
techniques to analyze facial expressions based on the Facial Action
Coding System (FACS). FACS measures facial expressions using 46
anatomically based component movements and has been used in many studies
by Kenneth Craig, PhD, a professor of psychology at the University of
British Columbia, a world renowned pain expert, and one of the study’s
co-authors.
The use of FACS in the past has allowed for identification of
pain-related facial movements, but this project took facial movement and
pain analysis one step further. In the software prototype, the study’s
authors translated the facial movement data into a pain score and then
compared that with the information collected from the child’s
self-reporting and the parent and nurse by proxy pain estimations.
“The software demonstrated good-to-excellent accuracy in assessing
pain conditions,” said Huang. “Overall, this technology performed
equivalent to parents and better than nurses. It also showed strong
correlations with patient self-reported pain ratings.” The software also
did not demonstrate bias in pain assessment by ethnicity, race, gender,
or age in the patient cohort studied.
Since the instrument is capable of “operating in real-time and
continuously,” using this approach to alert clinicians to instances of
pain at the time they occur instead of during scheduled assessments
might enhance efficient, timely allocation of pain interventions, noted
Huang. Furthermore, such technology could potentially advocate for youth
in pain when their parents are unavailable to notify medical staff
regarding their child’s pain level.
Huang said the approach requires further investigation with other
forms of clinical pain and across the broad age range of children. “It
still needs to be determined whether such a tool can be easily
integrated into clinical workflow and thus add benefit to current
clinical pain assessment methods and ultimately treatment paradigms,”
she said.
Coauthors include Karan Sikka, Alex Ahmed, and Damaris Diaz, UCSD; and Matthew Goodwin, Northeastern University.