Saint-Louis: Whether made by the body or ingested through diet, cholesterol plays a
vital role in cells. Cholesterol also is a building block of steroids
and hormones, including those that trigger puberty and support
pregnancy. A new study implicates a surprising regulator of cholesterol
in cells’ ability to make these hormones, especially in tissues
associated with fertility, such as the ovaries.
The researchers who conducted the study, at Washington University School of Medicine
in St. Louis, said the findings have potential implications for
investigating causes of infertility and understanding possible drivers
of the trend toward earlier onset puberty, particularly in girls.
The study appears in the June issue of the journal Cell Metabolism.
“Disruptions in the pathway we identified may have real implications
for fertility,” said senior author Daniel S. Ory, MD, the Alan A. and
Edith L. Wolff Distinguished Professor of Medicine. “Too much of a key
molecule we identified would likely impair proper steroid hormone
production and lead to infertility. Conversely, too little of it could
lead to premature sexual maturation.”
Studying mice, the researchers found that the key molecule — a
small strand of RNA — appeared in high levels in the ovaries and
testes, parts of the body that manufacture steroid hormones like
progesterone and testosterone. RNA is chemically similar to DNA but
serves different functions.
In the new study, Ory and his colleagues, including collaborator Jean
E. Schaffer, MD, the Virginia Minnich Distinguished Professor of
Medicine, showed that levels of this small RNA in healthy mice are high
at birth and gradually decrease. At about eight weeks, when the mice
reach sexual maturity, levels are very low, which dials up the
production of steroid hormones.
“The ovaries need to make steroids to support pregnancy when the mice
reach sexual maturation,” Ory said. “So we think this small RNA is at
least one of the regulators of the processes that govern when a mouse
becomes fertile.”
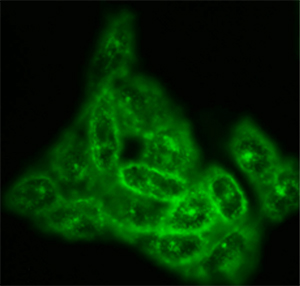
In hamster ovary cells deficient in this RNA, the investigators found
that cholesterol was directed into the cell’s energy factories called
mitochondria. Mitochondria are well known for making the fuel required
for cellular activities. But mitochondria also are responsible for
manufacturing steroids, starting with cholesterol as a raw material.
When cells have less of this RNA, cholesterol is channeled into the
mitochondria, where it is used as raw material to build steroids.
Conversely, when cells have too much of this RNA, cholesterol doesn’t
make it to the mitochondria, and without the raw material, mitochondria
can’t manufacture steroids.
The researchers also showed they could interfere with this RNA in
otherwise normal mice that had not yet reached sexual maturity. This
allowed cholesterol to be channeled into the mitochondria and triggered
steroid production in the mouse ovaries.
“We have not yet investigated whether these mice could breed
earlier,” Ory said. “But we certainly increased levels of pregnenolone
and progesterone, which are steroids necessary to support pregnancy.”
Ory said future work will investigate more details of how this RNA
interacts with proteins to increase or decrease cholesterol trafficking
into mitochondria and subsequent steroid production.
The RNA implicated in the study is surprising, according to Ory,
because it is classified as a small nucleolar RNA, or snoRNA, which has
important roles in helping cells manufacture proteins. But they are not
widely known for having other functions, such as encouraging the
production of steroids.
“That this snoRNA has a role in how the body meets the metabolic
demands of reproduction at a key time in the organism’s life is not
something we would have ever dreamed up,” Ory said. “This is one of
several hundred snoRNAs. Clearly, some of them have functions beyond the
traditional understanding of snoRNAs, and perhaps they should be
studied more systematically.”
The study also invites new ways
to look at influences on fertility and puberty such as chemicals in the
environment that mimic hormones.
“There are environmental cues that might be involved,” Ory said. “We
need to work with our colleagues in fertility research as we think about
future directions for this work.”