RSNA: A new MRI study has found distinct injury patterns in the brains of
people with concussion-related depression and anxiety, according to a
new study published online in the journal Radiology. The findings may lead the way to improved treatment and understanding of these common disorders, researchers said.
Post-concussion psychiatric disorders like depression, anxiety and
irritability can be extremely disabling for those among the nearly 3.8
million people in the United States who suffer concussions every year.
The mechanisms underlying these changes after concussion—also known as
mild traumatic brain injury—are not sufficiently understood, and
conventional MRI results in most of these patients are normal.
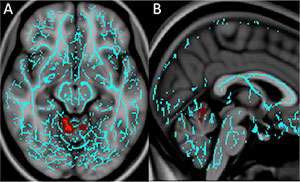
For the new study, researchers from the University of Pittsburgh
Medical Center (UPMC) in Pittsburgh used diffusion tensor imaging (DTI),
an MRI technique that measures the integrity of white matter—the
brain's signal-transmitting nerve fibers—to see if injuries to the
nerves may be the root cause of these post-traumatic depression and
anxiety symptoms.
The researchers obtained DTI and neurocognitive testing results for
45 post-concussion patients, including 38 with irritability, 32 with
depression and 18 with anxiety, and compared the results with those of
29 post-concussion patients who had no neuropsychiatric symptoms.
"Using other concussion patients as our controls was a big advantage
of our study," said lead author Lea M. Alhilali, M.D., assistant
professor of radiology at UPMC. "When you are able to study a similar
population with similar risk factors, you get much more reliable
results."
The researchers saw unique white matter injury patterns in the
patients who had depression or anxiety. Compared to controls, patients
with depression had decreased fractional anisotropy (FA), a measure of
the structural integrity of white matter connections, around an area
near the deep gray matter of the brain that is strongly associated with
the brain's reward circuit.
"The regions injured in concussion patients with depression were very
similar to those of people with non-traumatic major depression
disorder," Dr. Alhilali said. "This suggests there may be similar
mechanisms to non-trauma and trauma-dependent depression that may help
guide treatment."
Anxiety patients had diminished FA in a part of the brain called the
vermis that helps modulate fear-related behaviors. Since the vermis has
not been associated with dysfunction in non-traumatic anxiety disorders,
this finding may indicate that different treatment targets are required
for patients with anxiety after trauma, the researchers said.
No regions of significantly decreased FA were seen in patients with irritability relative to the control subjects.
"There are two major implications for this study," Dr. Alhilali said.
"First, it gives us insight into how abnormalities in the brain occur
after trauma, and second, it shows that treatments for non-trauma
patients with neuropsychological symptoms may be applicable to some
concussion patients."
The study also raises the possibility that some people diagnosed with
non-traumatic depression may actually have experienced a subclinical
traumatic event at some point earlier in their lives that may have
contributed to the development of depression, she noted.
In the future, the researchers hope to compare DTI findings in
concussion patients with depression to those of people who have
non-trauma-related depressive disorders.