Unlike the insomniac subject (who knows how long a night can be), the pathological snorer considers him/herself like a « good sleeper » and generally reports no bad memories from his/her nights.
Identified since 1965 in obese and sleepy subjects , the Obstructive Sleep Apnea syndrome (OSA) has been defined in 1972 and its «revolutionary » treatment, which consists in keeping a positive air pressure in the upper airways, was found in 1981.
25 years later, more than 100.000 people enjoy, thanks to that, a normal life expectancy but it is estimated that there remain four times more sick people who need to be detected.
Nowadays, SAS screening remains late (and poorly codified); OSA poses though several problems: excessive sleepiness : fall of performance and risk of accidents...; pathological complications : infarctus, obesity, diabetes ...
Symptoms
during sleep: snoring apnea, body movements, startle arousal, nycturia, hypersialorrhea, bedwetting, nocturnal sweating, sleep walking.
during wake: sleepiness, unfitful sleep, morning headaches, accidents (at home, at work, traffic), depressive syndrome, hypnagogic hallucination,s automatic behaviours, memory disorders, impotence, libido disorders, behaviour disorders.
Sleep apnea-hypopnea syndrome
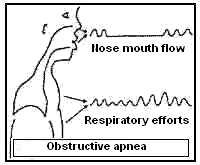
Pathological snoring must be detected during the interview of a subject who snores and is sleepy during the day ( Cf. Excessive Daytime Sleepiness), especially if there exist other factors of cardiovascular risks.Unlike simple snoring, it is often constant, occurs at sleep onset and presents, above all, numerous respiratory interruptions : Apneas.
Relatives describe these breaks very well, especially because the resumption of breathing is very noisy and is sometimes combined with important body movements (micro-arousals which give an idea of the sleepiness they induce).
- Sleep apnea (more than 50% of the time)
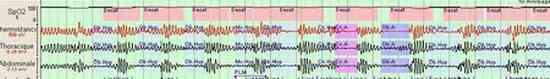
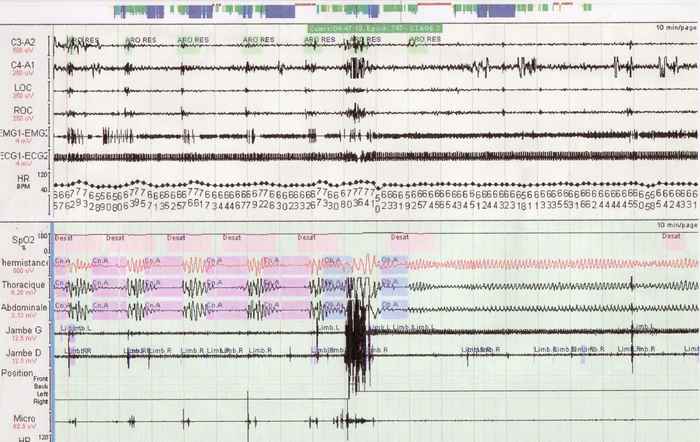
A polygraphic recording (and sometimes a polysomnography) of sleep is then necessary to complete diagnosis.
That examination is currently praticed in the sleep exploration units of most hospitals.
- "Sleep lab" (source http://www.medbo.de/555.0.html)

- Ambulatory polysomnography
UARS (Upper Airways Resistance Syndrome)
In the beginning of the illness, the subject who suffers from pathological snoring has to increase his/her muscular efforts in order to breathe.When the flow decreases, hypopnea is mentioned, which is a significant (more than 10 seconds) slowing down of the respiratory flow, combined with a lightening of sleep (arousal reaction) or with a micro-arousal, sometimes with discharges of limb movements.
When these efforts cause microarousals in a sufficient amount, the diagnosis of UARS (upper airways resistance syndrome) is carried out even if there are no significant desaturations yet (so far).
- Central hypopnea with crescendo
It must be noted that the subject often considers him/herself an excellent sleeper at that stage.
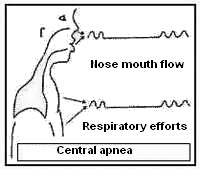
Central or Obstructive Apnea ?
- Central SAS w/ micro-arousal
Moreover, and without anybody knowing yet exactly why (several subgroups are distinguished), breathing interruptions, called "Central Apnea" because recordings show an abolition of the respiratory efforts (unlike the previous) also occur in some sick people.

- Central apnea with periodic desaturation
Some subjects have "mixed" or "complex" apnea : obstructive and central at the same time and more or less combined with hypopnea.
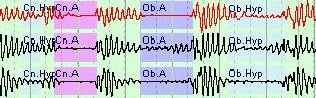
- Hypopnea + central apnea + obstructive hypopnea
The diagnosis of sleep apnea syndrome (SAS) makes no distinction between the different kinds of apnea.
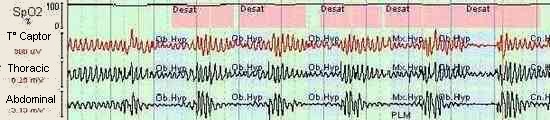
It relies on counting the number of events during one hour of sleep : the Apnea-Hypopnea Index (AHI).
An AHI is pathological if higher than 30, abnormal from 5/h.
The severity of the ventilatory disorder (especially if the index is comprized between 5 and 30) is estimated according to its consequences on the blood oxygene saturation (SpO2).

In all cases, breathing resumption occurs at the occasion of a lightening of sleep with a more or less long arousal reaction.
The amount of respiratory events is sometimes so important that some snorers no longer get any slow deep sleep.
Recordings allow to number and measure precisely the arousal phases which match breathing difficulties.

It is not rare to meet sick people who add up several hours of apnea during one night.
Some apneas last several minutes and only end when hypoxia (which can go down to less than 70% of normal) causes a reaction of arousal, which allows the resumption of voluntary breathing.
NB Often, the sleeper keeps no memory of these micro-arousal of respiratory origin.
(On the contrary, his/her naps satisfy him/her and, in the evenings, he/she falls asleep in less than five minutes !).
That situation sometimes dramatically delays diagnosis.
Medical complications of SAS

- Apnea and micro-arousal
- Repeated sleep fragmentation causes a chart of sleep insufficiency which main sign is an «Excessive Daytime Sleepiness» (EDS).
It is sometimes very important while the subject is not always aware of it because a certain amount of prejudices against sleep and the nap are the reason of an important diagnosis delay.
Many sick people live their daily life despite episodes of daytime sleepiness which sometimes carry along heavy consequences (statistics about traffic or work accidents have proven it for years).
In our opinion, the systematic pratice of the nap (in an adult who sleeps at night) should lead to a somnological checkup. - The other clinical signs are less specific but may draw the attention on the possibility of that sort of disorder.
- «Classically», morning headaches, combined with a delay to start off.
- Problems with "tiredness" are mentioned (because the subject diminishes his/her activity), as well as an impaired concentration.
In fact, they are not constant and the EDS induced is often masked or tolerated by the sick person. - Sleep fragmentation may favour parasomnias (Cf. "parasomnias").
- Two atypical clinical expressions can lead to diagnosis errors:
- pseudo-psychiatric chart: depression, dementia ...:
The accumulated consequences of tiredness and sleepiness sometimes have severe repercussions on the intellectual and sexual functions.
In accordance with the subject’s age and his/her degree of exhaustion, depression or dementia of Alzheimer type are sometimes mentioned erroneously in front of a complaint of memory and concentration disorder in a subject who snores and "has always had naps". - pseudo-prostatic chart.
The sleep of the pathological snorer is almost always interrupted by the
need to urinate. The excessive nocturnal diuresis (pollakiuria) is due
to changes in several hormones which limit diuresis during sleep. [3]
Nb. These arousals are remarkable because they are not
followed by insomnia, to the opposite of the constant micturitions about
which a bad sleeper who cannot go back to sleep complains.
In the beginning, the still young subject thinks that it is normal to get up to urinate (and sometimes to drink) several times over the night. But when the age of "prostate" comes, the part of an SAS in a "nocturnal pollakiuria" is not taken enough into account. It is not rare that a prostatic obstruction is blamed (sometimes with a surgical intervention "of convenience") for the embarrassment of someone who has to fraction his sleep in order to empty his bladder.
- pseudo-psychiatric chart: depression, dementia ...:
- The falls of blood oxygene saturation favour and aggravate cardio-vascular diseases (hypertension, infarctus...) and are often the cause of their accute decompensation during sleep (in case of a cardiac rhythm disorder, for example).
- An excess of insuline occurs which increases the risk of diabetes and obesity (by "hyper-insulinism").
It has, besides, been demonstrated that sleep deprivation is a risk factor for obesity (in particular during childhood) in itself which makes up a vicious circle. The links between sleep and weight are not yet all elucidated but "hypocretins" and "leptins" are hormones which offer important paths for investigation. - The stimulation of a cardiac hormone (Auricular Natriuretic Factor) causes a hypertensive reaction which adds itself up to the lack of ADH (fall of that anti-diuretic hormone caused by the disappearance of slow deep sleep) to induce an important nocturnal pollakiuria (the need to urinate and drink at night with a "weird" snoring in a sleeper very much evokes a SAS.
Consequences of sleep fragmentation :
Consequences of hypoxia:
Oxygene deprivation resulting from apnea leads, sooner or later, to metabolic and cardio-vascular disturbances.Diagnosis :
Currently, there exist diagnosis criteria based on sleep recordings.It is simple polygraphy which is more and more practiced in France, in particular by pneumologists, with an automatic reading of the respiratory recordings and of blood oxygene saturation. Ambulatory recordings (at the sick person’s home) are more and more easy to carry out.
Polysomnography (PSG) requires a visual analysis of the curve by a trained operator in order to determine the consequences of apnea and, most of all, hypopnea, on sleep. It is more tedious to carry out but can also be put up at the patient’s home.

- Ambulatory PSG
Treatment :
It relies, first of all, on the great hygienic and dietetic principles.If it is the case, it must be insisted on the aggravating effect of overweight (and of physical inactivity), alcohol, tobacco as well as medications (sedatives, beta-blockers and others).
The surgical removal of the uvula and palate (Uvpp) and sclerosis (with ultra-sounds) of the pharynx have not proven an unquestionable efficiency on the long course.
NB. In the child, though, it can be very useful to proceed to the removal of hypertrophied tonsils which can be an important hindrance in the airways.
Sometimes, it can happen that growth delays are caught up (because of an increase in growth hormone secretion) or a stop of bedwetting may occur.

Except for a few exceptions, pathological snoring has no other efficient treatment than the wearing of a respiratory mask all over the night.
That treatment, called Continuous Positive Airway Pressure (CPAP) has been considered to be revolutionary since 1981 (with the work of Sullivan, an Australian physician).
According to the type of apnea (central, obstructive or mixed (combined), there exist several types of devices offered by service companies and paid back by the Public Welfare System offices.

- CPAP device

- BiPAP device
Some systems, designed to slightly modify pharyngial space are under evaluation.

It consists in moulded to measure silicone devices which discretely push the jaw forward, thereby favouring the passing of the air in the pharynx during sleep.

These "mandibular advancement orthesis" (MAO) are adapted by authorized dentists and have the advantage of being often better accepted, particularly in younger patients. They have won an award in 2005 by the French therapeutic innovation agency (ANVAR).
Their result currently seem to be interresting in some sick people but not constant in others. Numerous studies are ongoing to specify their uses.
