“These patients do not have a lot of treatment options. There’s a tremendous need for therapies that work in this setting,” said Andrea Apolo, M.D., in the Genitourinary Malignancies Branch of NCI’s Center for Cancer Research.
By binding to a protein called PD-1 on the surface of T cells—a type of white blood cell—and preventing it from interacting with the PD-L1 protein on cancer cells, nivolumab releases the brakes on the immune system, allowing T cells to attack cancer cells.
“The approval of nivolumab is an affirmation of the important role that immunotherapy plays in the treatment of advanced bladder cancer,” Dr. Apolo said.
Clinical Study of Nivolumab
The approval was based on the results of a phase II clinical trial of 270 patients with unresectable locally advanced or metastatic bladder cancer that had worsened or come back after treatment with at least one platinum-based chemotherapy regimen.All patients in the trial were treated with the same dose of nivolumab. Of the 265 patients that could be evaluated, 52 (19.6%) had a confirmed objective response, meaning their tumors shrank measurably. Of those patients, 46 had a partial response and six had a complete response.
This is an improvement compared with the 10-15% objective response rate historically observed among patients treated with second-line chemotherapy, the investigators noted.
In other clinical studies, expression of PD-L1 by tumor cells has been used to predict patient response to treatment with checkpoint inhibitors. The research team found that treatment with nivolumab produced measurable responses among patients with all levels of PD-L1 expression. For example, 28% of patients whose tumors were considered to have the highest PD-L1 expression and 16% of patients whose tumors had the lowest PD-L1 expression had an objective response.
However, it is not surprising that some patients with low PD-L1 expressing-tumors had responses to nivolumab, said Dr. Apolo.
“There are a lot of variables with the PD-L1 test, and the immune system is very dynamic,” she explained. “We can’t really say that PD-L1 is a perfect biomarker to predict response.”
The most common side effects of nivolumab treatment seen in the trial were fatigue and diarrhea, and the most common inflammation-related side effects were skin-related, including rashes. A total of 14 patients discontinued treatment with nivolumab due to toxic effects and there were three treatment-related deaths.
Implications for Patients
This study of nivolumab has some limitations, Dr. Apolo noted. For example, because it was a single-arm study, the efficacy of nivolumab was not compared directly with that of another treatment. In addition, the accelerated approval was based on the objective response rate, the study’s surrogate endpoint.“The clinical benefit, as reflected by the surrogate endpoints, should be verified or established in a randomized clinical trial,” Dr. Apolo said. Currently, there is an ongoing randomized trial testing nivolumab versus placebo in patients who have undergone surgery to have their bladder tumor removed.
However, because there are so few treatment options for patients with metastatic bladder cancer who do not respond to chemotherapy, some physicians began treating patients with nivolumab as soon as preliminary results from the phase II trial were reported at an oncology meeting in 2016. Now that the FDA has approved the treatment, health insurance is more likely to cover its cost, explained Dr. Apolo.
Opening the Door for Other Potential Treatments
Another checkpoint inhibitor, atezolizumab (Tecentriq®), was approved to treat bladder cancer last year.“The approval of atezolizumab opened the door for other checkpoint inhibitors to be tested in bladder cancer because it confirmed that bladder cancer cells can be recognized by the immune system,” said Dr. Apolo.
In addition to nivolumab and atezolizumab, she noted, several other checkpoint inhibitors, such as pembrolizumab (Keytruda®), avelumab, and durvalumab have shown similar activity in patients with bladder cancer that no longer responds to platinum-containing chemotherapy.
“Although we do see responses, it is only in a small subset of patients. In order to improve upon this, we’re focusing on immunotherapy combinations,” Dr. Apolo continued. For instance, she is leading a clinical trial that will test the combination of nivolumab plus a targeted therapy, cabozantinib, with or without the addition of another checkpoint inhibitor, ipilimumab (Yervoy®), in patients with advanced or metastatic bladder cancer.
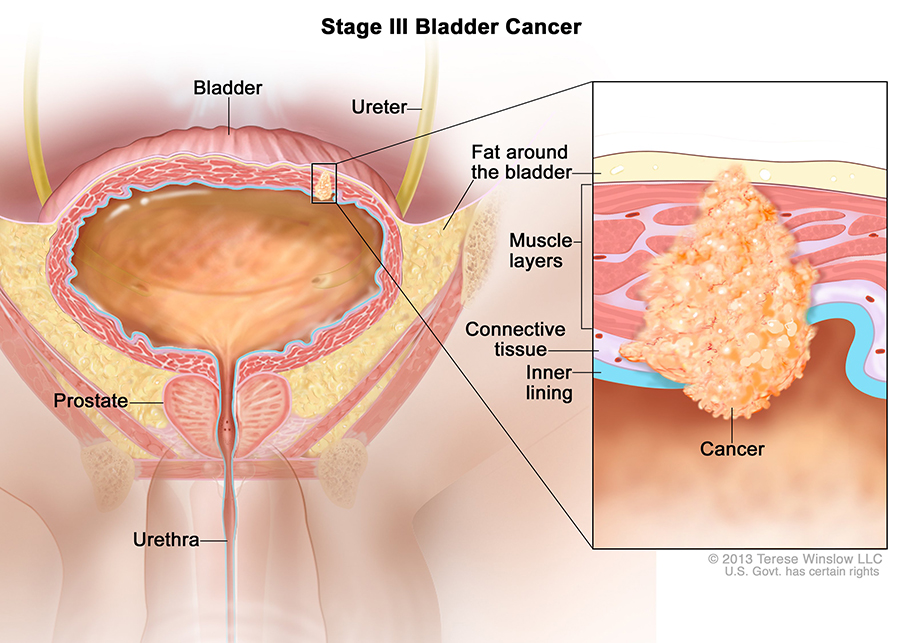
And several clinical studies are exploring the use of checkpoint inhibitors in earlier stages of bladder cancer, including as a first-line treatment for patients with metastatic disease, as an adjuvant therapy for patients with tumors that have spread locally into the surrounding muscle, and even for patients with very early-stage tumors that have not spread to the muscle.
“There are a lot of ongoing clinical trials right now. It’s a very exciting time,” Dr. Apolo said. “I think we are in a new era of treatment for bladder cancer.”