Mark Wilcox, Professor of Microbiology at the University of Leeds, led the study, which is published in the New England Journal of Medicine.
Professor Wilcox said: “About one in four patients who have been treated with antibiotics for an initial C.diff infection will go on to have a repeat infection.
“These repeat infections are more difficult to treat, have more severe outcomes for the patient, and are associated with more hospitalisations. It is important to treat the first episodes of C. diff infection optimally, as each recurrence increases the chance of another episode even more.
“Fewer recurrent infections would mean less need to use antibiotics, fewer hospital admissions, reduced costs for the NHS and possibly a reduction in deaths.”
For the study, doctors conducted a double-blind, randomised, placebo-controlled trial involving 2,655 adults across over 300 hospitals in 30 countries worldwide.
All the participants had primary or recurrent C.diff infections and were receiving standard-of-care antibiotics (metronidazole, vancomycin or fidaxomicin).
They were randomly assigned to receive infusions of:
- A single dose of (another human monocalonal antibody) actoxumab (10mg per kilogram of body weight)
- A single dose of bezlotoxumab (10mg per kilogram of body weight)
- Asingle dose of bezlotoxumab plus actotoxumab (10mg per kg of body weight)
- A placebo (saline)
After initial cure of their C.diff, the patients were then followed up for 12 weeks to see how many developed another C.diff infection.
- In the actoxumab group, 26% developed another C.diff infection
- In the bezlotoxumab group, 17% developed another C.diff infection
- In the bezlotoxumab/actotoxumab group, 15% developed another C.diff infection
- In the placebo group, 27% developed another C.diff infection.
“Doctors should now consider which patients could best benefit from use of bezlotoxumab,” said Professor Wilcox.
“The studies showed that bezlotoxumab was particularly effective in those patients with risk factors for poor outcome, including older age, immunocompromise, and severe infection.”
FURTHER INFORMATION
This research was supported by Merck.
To interview Professor Mark Wilcox, contact Sophie Freeman in the University of Leeds press office on 0113 343 8059 or email s.j.freeman@leeds.ac.uk
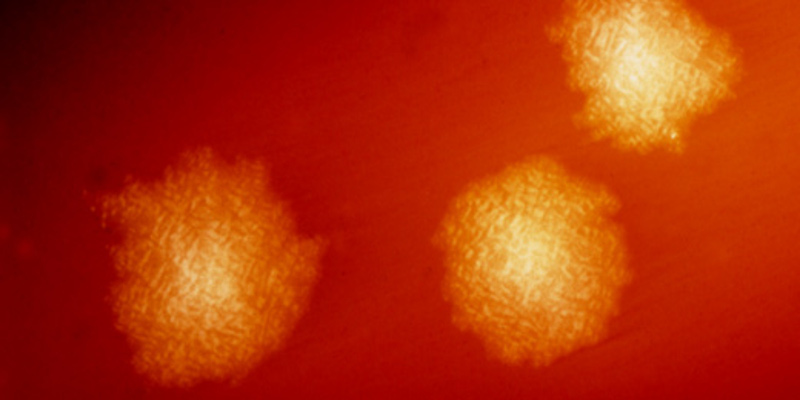
The image shows Clostridium difficile bacteria.