Pennsylvania: A new therapeutic agent tested in a mouse model of multiple sclerosis
(MS) produced anti-inflammatory activity and prevented loss of cells in
the optic nerve, according to a new study by researchers in the Perelman School of Medicine at the University of Pennsylvania, with Pittsburgh-based Noveome Biotherapeutics. The research was conducted in the laboratory of Kenneth Shindler, MD, PhD, an associate professor of Ophthalmology and Neurology, and published in Scientific Reports. The team demonstrated the therapeutic potential of the agent, called
ST266, for treating optic neuritis, inflammation that damages the optic
nerve and is a common presenting feature of MS. About half of patients
diagnosed with MS experience optic neuritis, which can cause mild to
moderate permanent loss of vision, but rarely complete blindness. ST266
is a solution of molecules that stimulate paracrine signaling. This is
one way in which cells “talk” to each other: One cell produces a
chemical signal that induces changes in nearby cells.
“In this case, the idea is that the many factors in ST266 not only
bind to cell receptors and cause changes within the cells they bind to,
but those cells then alter their own secretions and provide additional
signals to other neighboring cells, thus propagating an effect from a
relatively small amount of protein present in the therapy itself,”
Shindler said. “To the best of our knowledge, this study demonstrates,
for the first time, the ability to treat the optic nerve via the
intranasal route of administration.”
When ST266 was given to the MS mice via their nose, it reached the
central nervous system within 30 minutes and was detected at higher
concentrations in parts of the eye and optic nerve compared to other
areas of the brain. These findings demonstrated that this type of
delivery can target tissues of the eye, which is easier, less painful,
and less invasive than injecting medication directly into the eye.
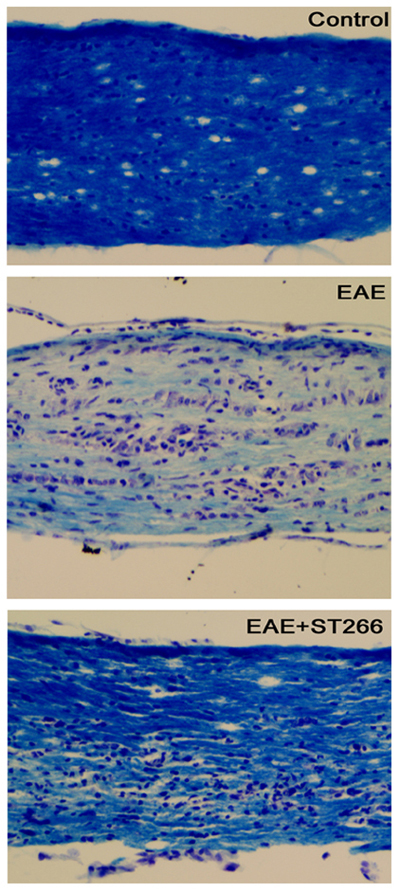
In mice with optic neuritis, the team showed that early treatment
with ST266 prevented damage and dysfunction, marked by significantly
reduced loss of optic nerve cells, and suppression of inflammatory cell
infiltration into the optic nerve. This in turn was associated with
limitation of the degree of demyelination caused by MS- related optic
neuritis. However, “it’s not known if these effects are independent
effects of the therapy or interdependent effects,” Shindler said.
Treatment of later-stage optic neuritis in the MS mice showed similar
results, resulting in improved visual function compared to untreated
groups. The data suggest that ST266 helps promote optic neuron survival
by potentially activating multiple pathways, including those that
prevent cell death.
“These results are particularly important as the preservation of
retinal cells is a significant factor when treating optic neuritis,”
Shindler said. “There is an increased need for combination treatment
options that are able to prevent nerve-cell axon loss for patients with
optic neuritis.”
Currently, the only acute treatment for MS-related optic neuritis is
IV steroids, which only hasten whatever amount of visual recovery will
occur even without treatment. Steroids do not prevent nerve damage or
permanent vision loss. “ST266's ability to preserve vision in the
preclinical model and reduce neuronal loss would be a huge advance if it
translates to human patients,” Shindler said.
The study also has implications beyond MS-related optic problems. “We
also showed an effect on cultured neurons, suggesting that effects may
translate to other optic nerve diseases, as well as other brain
neurodegenerative diseases,” Shindler said.
Editor’s Note: Dr. Shindler has served as a
scientific advisory board member and received consulting fees from
Noveome (formerly Stemnion, Inc.). In addition, Noveome has provided
unrestricted funds to Penn to support research in Dr. Shindler’s
laboratory.