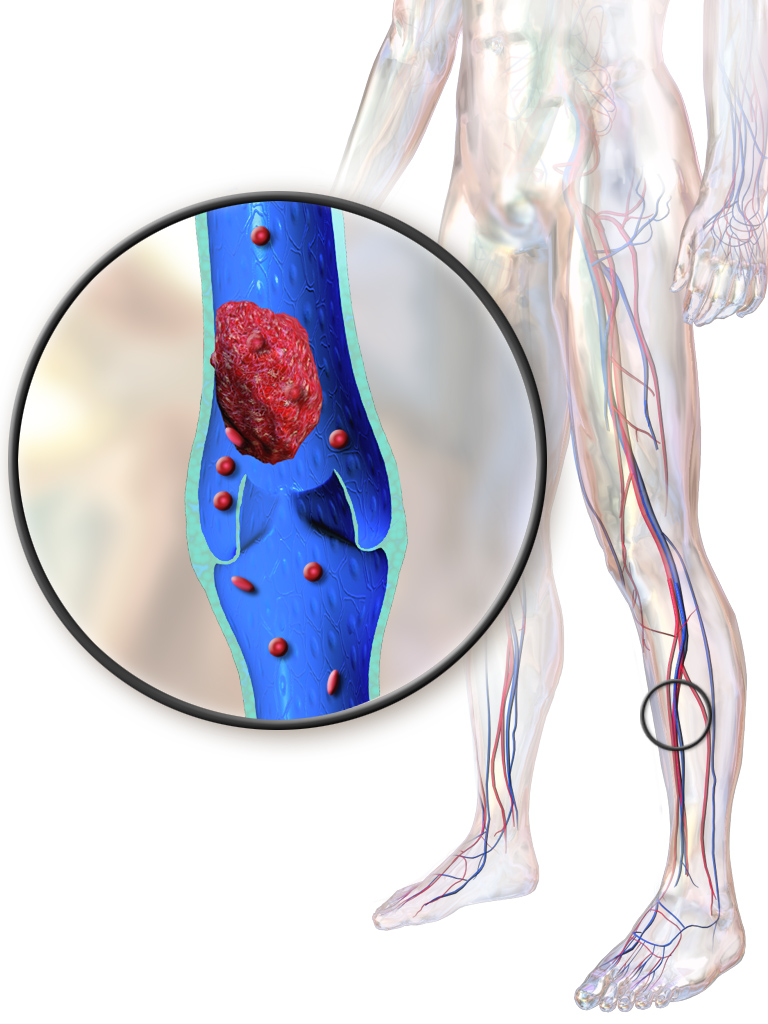
These thin the blood to reduce further clots from forming and prevent PE; yet PTS can still develop. Thrombolysis breaks down the blood clot. For DVT, drugs such as streptokinase, urokinase and tissue plasminogen activator are infused into a vein in the arm or foot or, in some cases, directly at the site of the clot using a catheter and X-ray control. Bleeding complications, stroke or intracerebral haemorrhage are potential harmful events for both treatments.
Study characteristics and key results
The review results are based on 17 controlled trials that randomised a total of 1103 people with acute DVT (within 21 days of onset of symptoms) to receive thrombolysis or anticoagulant treatment. Trials were carried out principally in the USA, Scandinavia, Germany and the UK. All trials included men and women ranging in age from 18 to 75 years with a preponderance of older adults.
The present review (current until February 2016) showed that thrombolysis may have advantages over standard anticoagulation treatment. Thrombolysis effectively dissolved the clot so that complete clot breakdown occurred more often with thrombolysis than with standard anticoagulant therapy. Blood flow in the affected vein (venous patency) was also better maintained. Three trials (306 participants) continued for over six months and found that fewer people developed PTS when treated with thrombolysis, 45% compared with 66% in the standard anticoagulation treatment group. Two trials (211 participants) which continued for over five years also showed that fewer people developed PTS when treated with thrombolysis.
Those receiving thrombolysis had more bleeding complications than with standard anticoagulation (10% versus 8%). Most bleeding episodes and deaths occurred in the older studies. Use of strict eligibility criteria appears to have improved the safety of this treatment, which is effective delivered directly to the clot by catheter or via bloodstream from another vein.
Qualitity of the evidence
Using GRADE assessment, the evidence was judged to be of moderate quality due to many trials having low numbers of participants. However, the results across studies were consistent and we have reasonable confidence in these results.
Authors' conclusions:
Thrombolysis increases the patency of veins and reduces the incidence of PTS following proximal DVT by a third. Evidence suggests that systemic administration and CDT have similar effectiveness. Strict eligibility criteria appears to improve safety in recent studies and may be necessary to reduce the risk
of bleeding complications. This may limit the applicability of this
treatment. In those who are treated there is a small increased risk
of bleeding. Using GRADE assessment, the evidence was judged to be of
moderate quality due to many trials having low numbers of participants.
However, the results across studies were consistent and we have
reasonable confidence in these results.