Liverpool: Microbiologists have identified how MRSA may be more effectively
treated by modern-day antibiotics, if old-fashioned penicillin is also
used. The team from the University of Liverpool and the National
University of Ireland Galway have shown that, although penicillin does
not kill the bacteria, it does weaken their virulence, making it easier
for our immune system and other antibiotics to eradicate the infection.
The research findings, funded by the Health Research Board and the Medical Research Council, are published in the Journal of Infectious Diseases.
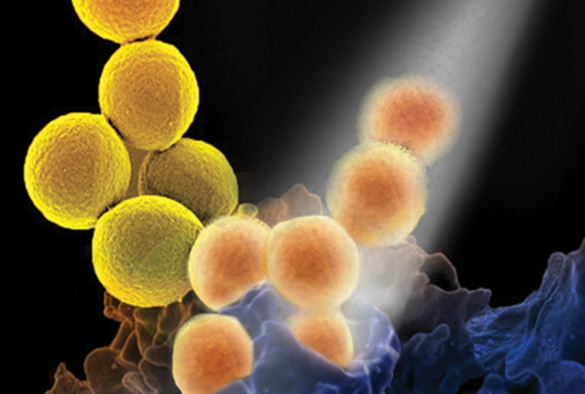
MRSA infection is caused by a type of Staphylococcal bacteria that
has become resistant to many of the antibiotics used to treat ordinary
infections. This results in significant morbidity and mortality with up
to 20% of patients infected with MRSA dying from systemic infections.
Escalating crisis
Study co-lead Professor Aras Kadioglu, from the University’s Institute of Infection and Global Health,
commented: “Although aggressive hospital infection control initiatives
appear to be having a positive impact on hospital-acquired MRSA rates in
some developed countries, the global burden still remains unacceptably
high. Infections caused by community associated MRSA strains and strains
that are currently methicillin sensitive are increasing at a worrying
speed. Given the escalating antimicrobial resistance crisis, it is
imperative to identify new therapeutic strategies and to re-evaluate how
current antimicrobial drugs are used, as such our data are timely and
highly important.”
Professor James O’Gara of the National University of Ireland Galway
commented: “Our findings explain the anti-virulence mechanism of
penicillin-type antibiotics and support the re-introduction of these
drugs as an adjunct therapeutic for MRSA infections. MRSA can be
extremely virulent, which is part of the challenge in treating it. Our
laboratory research shows that when exposed to penicillin, the bacteria
switches off its toxin genes and instead concentrates on thickening its
cell wall to resist the antibiotic. Our immune systems can then take
advantage of this compromised state to destroy the bacteria.”
Potential to change guidelines
This new treatment strategy for MRSA infections has the potential to
change the current clinical guidelines for treatment of patients with
MRSA infections in both hospital and community settings. A recent
randomised controlled trial in Australia involving 60 patients led by
Menzies School of Health Research showed that the beta-lactam antibiotic
flucloxacillin in combination with vancomycin significantly reduced the
duration of MRSA sepsis from 3 days to 1.9 days.
“The clinical findings in Australia are very important and now we
have the key laboratory data that help explain why the combination of
two antibiotics is better than one. The beauty of this approach is that
penicillin type antibiotics are not only widely available and safe, but
can potentially and more easily be included in clinical practice without
the need for long and expensive clinical trials needed for new drugs,”
added Professor O’Gara.
Graham Love, Chief Executive at the Health Research Board commented:
“This research demonstrates the potential payback having a vibrant
health research programme. It clearly has the potential to change
clinical practice and improve outcomes for patients.”
Antimicrobial resistance (AMR) is one of the greatest current threats
to human health. The recent report commissioned by the UK Government,
concluding that AMR infections will cause more deaths than cancer by
2050 if not addressed urgently.
The paper ‘Redeploying β-Lactam Antibiotics as a Novel
Antivirulence Strategy for the Treatment of Methicillin-Resistant
Staphylococcus aureus Infections’ is published in the Journal of Infectious Diseases and is available to view here.