“Having biomarkers for a disease is extremely important to evaluate the efficacy of experimental treatments,” said Craig McDonald, professor and chair of Physical Medicine and Rehabilitation at UC Davis School of Medicine and a principal investigator of the study. “This is especially important in Duchenne muscular dystrophy, in which only a few quantifiable measures currently exist.”
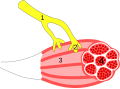
Duchenne muscular dystrophy is a recessive X-linked genetic disorder that affects about 1 in 3,600 boys worldwide (girls who carry a single mutation are usually not affected). A mutation in the dystrophin gene either reduces or eliminates activity of a structural protein that protects muscle from breakdown during normal activity. Without normal dystrophin, muscle cells are easily damaged, and muscle is progressively replaced by fat and fibrotic tissue. Symptoms of muscle weakness become apparent in early childhood; as the disease progresses, patients usually become wheelchair-dependent in their early teens, and typically die in their 20s of cardiac hypertrophy resulting from severe fibrosis of heart muscle.
The study compared the blood of 93 patients with Duchenne muscular dystrophy ages 2 to 29 years to blood from 45 age-matched healthy volunteers used as controls. Serum samples were analyzed using a sophisticated assay system that uses single strands of DNA or RNA molecules to selectively bind to proteins. More than 1,000 proteins were identified, and 44 were found that differed significantly in concentration between patient and normal samples: 24 were increased in patients and 20 were decreased.
The researchers found interesting patterns of the concentrations of biomarkers as a factor of patient age – an indicator of disease progression. For example, 18 proteins were present at much higher levels in the youngest patients than in healthy children of the same age, and then decreased with age in the patients while remaining the same or increasing slightly in the controls. The authors speculate that these proteins probably result from muscle damage and cell death: One would expect high levels in patients early in the course of the disease, then a decline over time because of diminishing muscle mass.
Other markers that were identified are associated with inflammation and could be used to monitor efficacy of anti-inflammatory medications used to treat the disease.
Clinical trials require objective measures to monitor the effects of a new therapy. For Duchenne muscular dystrophy, monitoring is currently commonly done with measures of muscle strength and clinical measures of function such as the six-minute walk test, which measures how far a child can walk in six minutes without stopping. Because the latter test depends on a child’s ability to walk, patients who are wheelchair dependent have been limited in their participation in clinical trials, so do not have access to promising new therapies. Very young children who are too unreliable to perform walking and muscle strength tests are also excluded, which according to McDonald, is especially problematic because of the desirability of beginning treatment at the earliest age possible.
“There have been revolutionary breakthroughs in novel therapeutics in recent years that target underlying disease processes, but more than half of patients are unable to participate in testing these drugs,” said McDonald, who directs UC Davis Health System’s Neuromuscular Disease Clinic and is an internationally recognized Duchenne muscular dystrophy expert. “Having validated biomarkers to assess the ability of new therapies to positively affect disease progression will be a game-changer and open up participation to everyone.”
McDonald expects that because biomarkers are a more sensitive measure of treatment effects than the traditional tests of walking and muscle strength, determining efficacy of new drugs should take only months instead of years. His UC Davis team, which has established one of the largest clinical-trials sites in the nation for Duchenne, will next focus on evaluating specific biomarkers in clinical trials to determine which can be used to reliably monitor treatment efficacy.
Results from this work are available to researchers and clinicians in the field of Duchenne muscular dystrophy to help incorporate biomarkers in to future clinical trials.
“We hope that experts in Duchenne muscular dystrophy can use biomarkers identified to accelerate the search for new diagnostic, prognostic and therapeutic approaches for this devastating disease,” said McDonald. “The same technology could also be fruitfully applied to many different rare muscle diseases.”
Research for this study was supported by the Department of Education/National Institute on Disability and Rehabilitation Research; the Department of Defense; the National Institutes of Health; the Parent Project Muscular Dystrophy; National Institutes of Health grants; The Clark Charitable Foundation; and partially by National Institutes of Health core grants.