Auckland: A research team from Auckland is trying to understand Huntington’s disease better and investigate differences
in genes and proteins, and brain cell development and function between
normal and Huntington’s disease patients using live human brain cells. “By doing this, we hope to identify cell targets that may lead to new
drug development,” says Dr Connor who is based in the University’s
Centre for Brain Research. “The last step of the project is
collaboration with Griffith University in Brisbane at the Eskitis
Institute that has a natural drug compound library of more than 200,000
compounds.
“If we can identify some targets in the live human Huntington disease
brain cells, we are going to use these cells to screen drugs,
potentially to identify new compounds that we could then take further
forward into drug development,” she says. “The beauty of that are these
targets and compounds will be tested on human cells, not on animal
cells or on engineered human cells lines. That will mean a much more
precise result and hopefully faster and more successful translation to
clinical use.”
In 2007 Shinya Yamanaka working at the University of Kyoto, developed
a unique cell technology that takes human skin cells (or fibroblasts),
and ’reprogrammes‘ them back to an embryonic-like stem cell state
(induced pluripotent stem cells). (Yamanaka was awarded the Nobel Prize
for this work in 2013).
That was an advance on using embryonic stem cells, but that approach
has the same issues as working with pluripotent stem cells. Both
embryonic stem cells and pluripotent stem cells are innately unstable -
they can turn into all different types of cells including the potential
to turn into cancer cells and cause tumours.
“On the one hand it's unique and exciting work because the
pluripotent skin cells can turn into all different cell and tissue
types, but we are looking for a clinical application,” says Dr Connor
“If you wanted to use those cells for cell or tissue replacement, the
pluripotency is an issue. We need to make sure that for clinical
application, the cells are at the mature stage where they lose that
pluripotency.”
"This is the issue that embryonic stem cell technology is facing and
the reason why it has not gone into the clinic as fast as everyone
thought," she says. “It's because nobody has yet managed to completely
purify these - the pluripotent cells of either the reprogrammed skin
cells or the embryonic stem cells.
“We want to work with brain stem cells that are multi-potent, so that
they will only turn into brain cells and so we are using a technology
called direct cell reprogramming.”
The first technology that was developed in direct reprogramming for
neuroscience was taking skin cells and directly turning them into mature
neurons.
"It's pretty incredible to go from one mature cell type to another,”
says Dr Connor. “The issue around that is of course that a mature cell
can’t proliferate at all. If you only get ten percent of your cells
turning into a mature neuron, then that’s all you have got to work with,
so it’s not very efficient and there are issues around how much
research you can do."
Dr Connor wanted something in between the two techniques and so she
and her team identified two genes which are involved in brain
development - one known as Pax6 (the first gene to come up during
development when the neural tube forms), and the other called Sox2
(which is also involved in forming brain cells and involved in stem cell
function as well).
"We have generated this technology now where we can put Sox2 and
Pax6 into adult human skin cells and generate brain stem cells which we
call neural precursor cells. From those cells we can generate different
types of mature brain cells. That’s taken us about three years to get
up and going.
“There are two areas where this research can be used. One is for
cell replacement therapy - replacing brain cells that have been lost
through disease- in this case brain diseases where there is a specific
population of cells lost, (such as Huntington’s and Parkinson’s disease)
and we can target that population of cells.”
The second area is to study neurological diseases to further
understand what causes them and potentially to identify new drug
targets.
“We can use skin cells from patients with genetic disorders such as
Huntington’s disease, because that genetic mutation is in all the cells
of that patient, but only shows up as a functional deficit in the brain
cells,” says Dr Connor.
“We can take those cells from a simple skin biopsy and we can
reprogramme them using Sox2 and Pax6 to become a brain stem cell,” she
says. “Our preliminary data already shows that we can compare brain
stem cells from a patient with Huntington’s disease to a patient who is
neurologically normal and detect differences.
“We have seen right from the start of brain stem cell development,
that there are already genetic defects,” says Dr Connor. “Some cells
are already altered, even at that early stage of development.
“Although Huntington’s disease is a genetic disorder, you tend not
to see the onset until patients are about 40-50 years old, so it’s a
disease we see later in life,” says Dr Connor. “However the genetic
changes are there and the cells are impaired, right from the word go.
“This reprogramming process starts to give us an idea about what the
mutation is doing in the developing cell,” she says. “We also see how
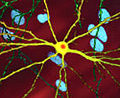
the cell matures and how it functions. These live human brain cells
give us the capability of observing this development, and also to
observe the function and vulnerability of live human GABAergic medium
spiny neurons which are the ones that are lost in Huntington’s disease.”
“In our preliminary work using reprogrammed brain stem cells
generated from Huntington’s disease patients, we showed that there are
some genes in Huntington’s disease that were hugely over-expressed
compared to neurologically-normal subjects”, says Dr Connor. “They are
genes that are also involved in forming a mature GABAergic neuron,
suggesting the development process in Huntington’s disease was altered
and the cells may be maturing too fast.
She says this technology enables her team to look at the disease
pathogenesis – something they can’t do specifically in humans until
now.At present, the only technology researchers can do that with is
transgenic animals or zebrafish. The only human material they could use
is post mortem human tissue which is usually at an end-stage usually.