Johns Hopkins: More than 30,000 people in the U.S. are diagnosed with Lou Gehrig’s disease, or amyotrophic lateral sclerosis (ALS).
Johns Hopkins researchers have transformed skin cells donated by ALS
patients into brain cells affected by the progressive, fatal disease.
The resulting cell library is being used by researchers worldwide in the quest for better ALS treatments.
Researchers at Johns Hopkins Medicine have transformed skin cells from
patients with Lou Gehrig’s disease, or amyotrophic lateral sclerosis
(ALS), into brain cells affected by the progressive, fatal disease and
deposited those human-made cells into the first public ALS cell library,
enabling scientists to better study the disease.
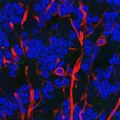
Using a genetic engineering technique that causes adult skin cells to
transform into “pluripotent” cells, otherwise known as induced
pluripotent stem cells, which can take the form of many different cells
found in other parts of the body, “we make brain cells out of the
patient’s own skin,” says Jeffrey Rothstein, M.D., Ph.D., who directs the Brain Science Institute and the Robert Packard Center for ALS Research.
While the technique for creating these human-made cells has been used
by other researchers, Rothstein and his colleagues are the first to use
these induced pluripotent stem cells to create the largest library of
brain cell lines donated voluntarily by more than 20 ALS patients whose
disease was caused by various genetic mutations. “These human cellular
tools will serve as a platform to understand ALS and someday discover
new drugs to treat our patients,” says Rothstein, senior author of a study about the work, which was recently published online in PLOS ONE.
More than 30,000 people in the U.S. are diagnosed with ALS. Men appear
to be affected slightly more than women. One of every 500 deaths in men
is due to ALS, says Rothstein, “so just about everyone is going to know a
neighbor, friend or family member who will eventually succumb to this
terrible disease.”
There is no known cure for ALS and only one FDA-approved drug,
riluzole, which may only add a year to a patient’s life span, says
Rothstein.
Since the 1990s, researchers have studied the disease and its potential
treatments in mice. The mouse model looks very much like what happens
in people, Rothstein says, “but after 25 years, it has not led to the
development of a drug that works in our patients.” A handful of drugs
were effective in mice and passed phase II clinical trials, which
establish a drug’s safe dosage for humans, but they all failed phase III
trials, which confirm a drug’s effectiveness in people.
“There has to be a sea change in how we approach ALS,” Rothstein says.
Because there is no ethical or simple way to obtain brain tissue from
living ALS patients, Rothstein and colleagues turned to induced
pluripotent stem cell production. The technique gives researchers a tool
to look at diseased human brain cells, including specialized nerve
cells called astroglia, which play a critical role in ALS progression.
Rothstein and his team created 22 patient-specific cell lines that
included some common mutations known to be associated with ALS and
deposited them in a cell library, to be shared with other scientists.
The library includes cells from patients with inherited ALS, which
accounts for about 10 percent of ALS cases. Rothstein and his team also
have generated cells from patients with the noninherited form of the
disease — sporadic ALS,
which makes up 90 to 95 percent of ALS cases. From one patient, the
researchers collected a genetic variant found in both inherited and
sporadic forms of the disease, and they added that variant to the
library.
Many scientists around the world have already used the library, and
Rothstein hopes it will grow, with researchers making deposits of their
own patients’ cell lines. Eventually, induced pluripotent stem cells may
be used to model diseases other than ALS and to test potential drug
treatments, says Rothstein, who adds: “Now we have a real model for
what’s wrong with my patients.”