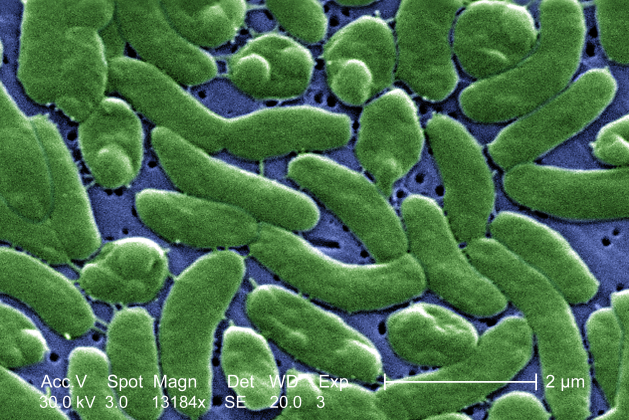
CDC. US: Vibrio vulnificus is a bacterium in the same family as those that cause cholera and Vibrio parahaemolyticus. It normally lives in warm seawater and is part of a group of vibrios that are called "halophilic" because they require salt.
V. vulnificus can cause disease in those who eat
contaminated seafood or have an open wound that is exposed to
seawater. Among healthy people, ingestion of V. vulnificus
can cause vomiting, diarrhea, and abdominal pain. In immunocompromised
persons, particularly those with chronic liver disease, V. vulnificus
can infect the bloodstream, causing a severe and life-threatening
illness characterized by fever and chills, decreased blood pressure
(septic shock), and blistering skin lesions. V. vulnificus bloodstream infections are fatal about 50% of the time.
V. vulnificus can cause an infection of the skin when
open wounds are exposed to warm seawater; these infections may lead to
skin breakdown and ulceration. Persons who are immunocompromised are
at higher risk for invasion of the organism into the bloodstream and
potentially fatal complications.
V. vulnificus is a rare cause of disease, but it is also underreported. Between 1988 and 2006, CDC received reports of more than 900 V. vulnificus infections from the Gulf Coast states, where most cases occur. Before 2007, there was no national surveillance system for V. vulnificus,
but CDC collaborated with the states of Alabama, Florida, Louisiana,
Texas, and Mississippi to monitor the number of cases of V. vulnificus infection in the Gulf Coast region. In 2007, infections caused by V. vulnificus and other Vibrio species became nationally notifiable.
Persons who are immunocompromised, especially those with chronic liver disease, are at risk for V. vulnificus
when they eat raw seafood, particularly oysters. A recent study
showed that people with these pre-existing medical conditions were 80
times more likely to develop V. vulnificus bloodstream
infections than were healthy people. The bacterium is frequently
isolated from oysters and other shellfish in warm coastal waters
during the summer months. Since it is naturally found in warm marine
waters, people with open wounds can be exposed to V. vulnificus through direct contact with seawater. There is no evidence for person-to-person transmission of V. vulnificus.
V. vulnificus infection Is diagnosed by stool, wound, or blood
cultures. Notifying the laboratory when this infection is suspected
helps because a special growth medium should be used to increase the
diagnostic yield. Doctors should have a high suspicion for this
organism when patients present with gastrointestinal illness, fever,
or shock following the ingestion of raw seafood, especially oysters,
or with a wound infection after exposure to seawater.
If V. vulnificus is suspected, treatment should be
initiated immediately because antibiotics improve survival. Aggressive
attention should be given to the wound site; amputation of the
infected limb is sometimes necessary. Clinical trials for the
management of V. vulnificus infection have not been
conducted. The antibiotic recommendations below come from documents
published by infectious disease experts; they are based on case reports
and animal models.
- Culture of wound or hemorrhagic bullae is recommended, and all V. vulnificus isolates should be forwarded to a public health laboratory
- Blood cultures are recommended if the patient is febrile, has hemorrhagic bullae, or has any signs of sepsis
- Antibiotic therapy:
- Doxycycline (100 mg PO/IV twice a day for 7-14 days) and
a third-generation cephalosporin (e.g.,ceftazidime 1-2 g IV/IM every
eight hours) is generally recommended
- A single agent regimen with a fluoroquinolone such as
levofloxacin, ciprofloxacin or gatifloxacin, has been reported to be
at least as effective in an animal model as combination drug regimens
with doxycycline and a cephalosporin
- Children, in whom doxycycline and fluoroquinolones are
contraindicated, can be treated with trimethoprim-sulfamethoxazole
plus an aminoglycoside
- Necrotic tissue should be debrided; severe cases may require fasciotomy or limb amputation
V. vulnificus infection is an acute illness, and those who recover should not expect any long-term consequences.
Although oysters can be harvested legally only from waters free from
fecal contamination, even legally harvested oysters can be
contaminated with V. vulnificus because the bacterium is naturally present in marine environments. V. vulnificus does not alter the appearance, taste, or odor of oysters. Timely, voluntary reporting of V. vulnificus
infections to CDC and to regional offices of the Food and Drug
Administration (FDA) will help collaborative efforts to improve
investigation of these infections. Regional FDA specialists with
expert knowledge about shellfish assist state officials with
tracebacks of shellfish and, when notified rapidly about cases, arez
able to sample harvest waters to discover possible sources of
infection and to close oyster beds when problems are identified. Ongoing
research may help us to predict environmental or other factors that
increase the chance that oysters carry pathogens.
Some tips for preventing V. vulnificus infections, particularly among immunocompromised patients, including those with underlying liver disease:
- Do not eat raw oysters or other raw shellfish.
- Cook shellfish (oysters, clams, mussels) thoroughly.
- For shellfish in the shell, either a) boil until the shells
open and continue boiling for 5 more minutes, or b) steam until the
shells open and then continue cooking for 9 more minutes. Do not eat
those shellfish that do not open during cooking. Boil shucked oysters
at least 3 minutes, or fry them in oil at least 10 minutes at 375°F.
- Avoid cross-contamination of cooked seafood and other foods with raw seafood and juices from raw seafood.
- Eat shellfish promptly after cooking and refrigerate leftovers.
- Avoid exposure of open wounds or broken skin to warm salt or brackish water, or to raw shellfish harvested from such waters.
- Wear protective clothing (e.g., gloves) when handling raw shellfish.