Symptoms
The symptoms particularly depend on which part of the brain is affected. The following are common signs of a stroke:
sudden weakness, numbness and signs of paralysis, speech problems,
trouble seeing, dizziness and difficulty walking, severe headache.
A stroke is an emergency. If you think someone might be having a stroke, it is essential that you call the emergency services (in Germany: 112, in the United States: 911, 999 in UK) immediately and ask for medical help.
Reacting quickly and getting treatment as soon as possible can sometimes stop brain cells from dying. That lowers the risk of serious consequences and can also keep symptoms to a minimum.
Typical symptoms of a stroke include:
People who are having a stroke need to go to hospital to have appropriate tests done and get the right treatment. And no-one will blame you if it turns out to be a "false alarm".
A stroke is an emergency. If you think someone might be having a stroke, it is essential that you call the emergency services (in Germany: 112, in the United States: 911, 999 in UK) immediately and ask for medical help.
Reacting quickly and getting treatment as soon as possible can sometimes stop brain cells from dying. That lowers the risk of serious consequences and can also keep symptoms to a minimum.
Typical symptoms of a stroke include:
- Sudden weakness, numbness and signs of paralysis: People who are having a stroke can often no longer move their arm, hand and/or leg properly. As well as weakness, some people experience sensations like tingling and numbness. It can sometimes feel like your arm or foot has gone to sleep. Drooping on one side of the mouth is another typical sign of a stroke. These symptoms usually just affect one side of the body, and only rarely both sides.
- Speech problems: A lot of people suddenly have difficulties finding the right words during a stroke and speak in broken sentences. Sudden slurring of words or mumbling can also be signs of a stroke. Sometimes people have problems understanding what others are saying – although they can hear the words, they cannot make sense of them.
- Vision problems: A stroke can affect vision. People are then no longer aware of things to one side of their body, and their field of vision in the left or right eye is limited. Many people suddenly have double vision. If they want to reach for something, such as a cup, they often miss it.
- Dizziness and trouble walking: People may have difficulty keeping their balance. They either feel like everything is spinning around or swaying from side to side.
- Severe headache: A sudden, unusually strong headache can also be a sign of a stroke. Such headaches are caused by acute blood supply problems in the brain or by bleeding in the brain due to a torn or burst blood vessel. Headaches may be the only symptom at first, followed a little later by other symptoms such as paralysis and confusion. Nausea and vomiting are also possible symptoms.
Award-winning video, the original "Stroke Heroes Act FAST" animation, uses a catchy tune to help people remember the signs and symptoms of stroke - and stresses that the only response to even a single sign of stroke is an immediate call to 9-1-1.
Information needed by paramedics
When somebody is having a stroke, they are often unable to communicate, or only with difficulty. So it is important that other people who notice that something is wrong clearly describe the symptoms, the circumstances and, if possible, any previous medical conditions. The following information is particularly important:- When did the symptoms begin?
- What was the person doing when the symptoms started? For example, were they doing something strenuous?
- Which signs of a stroke did they have and how did things develop?
- Are they currently taking any medication?
- Do they have any known cardiac arrhythmias (heart rhythm problems), in particular atrial fibrillation?
- Have they had similar symptoms or treatment for a stroke in the past?
People who are having a stroke need to go to hospital to have appropriate tests done and get the right treatment. And no-one will blame you if it turns out to be a "false alarm".
Causes
There are two main causes of a stroke.
They are most frequently caused by a blood clot that is blocking a
blood vessel in the brain. These clots can form in the brain itself, for
example because of changes in the artery wall caused by infection.
However, they occur more often in another part of the body and are
carried into the brain along the bloodstream, where they then block a
blood vessel. A stroke that is caused by a blocked blood vessel is referred to as an ischemic stroke.
Bleeding (hemorrhage) in the brain is the second, less common cause. This can occur because a blood vessel ruptures and blood leaks into the brain tissue.
In both cases, part of the brain is temporarily or permanently no longer supplied with enough oxygen. The sooner oxygen supply is restored, the better the chances are of keeping damage to a minimum.
Bleeding (hemorrhage) in the brain is the second, less common cause. This can occur because a blood vessel ruptures and blood leaks into the brain tissue.
In both cases, part of the brain is temporarily or permanently no longer supplied with enough oxygen. The sooner oxygen supply is restored, the better the chances are of keeping damage to a minimum.
Risk factors
It is very uncommon for blood clots to develop in the blood vessels
of healthy people. But certain illnesses and genetic factors can
increase the risk of a stroke. They include high blood pressure and long term atrial fibrillation.
It is possible that the typical symptoms of a stroke go away by themselves after a few hours. This could be a "transient ischemic attack" (TIA), where a blood clot had formed and then went away again before the brain was damaged more severely. A TIA is however an indication of an increased risk of a stroke.
It is possible that the typical symptoms of a stroke go away by themselves after a few hours. This could be a "transient ischemic attack" (TIA), where a blood clot had formed and then went away again before the brain was damaged more severely. A TIA is however an indication of an increased risk of a stroke.
Frequency and outlook
Around one out of 1,000 people has a stroke in their lifetime. The risk increases with age: Around 20 out of 1,000 people aged over 85 are affected.
Most people survive a stroke. But strokes can cause paralysis in certain parts of the body or problems with various bodily functions, for example speech.
Symptoms such as paralysis often get better over time, but they can also be permanent. Psychological problems like depression are therefore not uncommon.
People who have had a stroke are also at greater risk of having another one. Around 40 out of 100 people who survive an ischemic stroke have another stroke within ten years.
The risk is particularly high within the first six months. But people who have had a stroke are also more likely to have other cardiovascular diseases such as a heart attack.
Most people survive a stroke. But strokes can cause paralysis in certain parts of the body or problems with various bodily functions, for example speech.
Symptoms such as paralysis often get better over time, but they can also be permanent. Psychological problems like depression are therefore not uncommon.
People who have had a stroke are also at greater risk of having another one. Around 40 out of 100 people who survive an ischemic stroke have another stroke within ten years.
The risk is particularly high within the first six months. But people who have had a stroke are also more likely to have other cardiovascular diseases such as a heart attack.
Diagnosis
Somebody having a stroke requires urgent medical attention. If you think you or somebody else might be having a stroke you should call for an ambulance immediately (112 in Germany; 911 in the U.S, 999 in UK.). Do not wait to see if the symptoms go away.
After the paramedics have provided first aid, the patient will be taken to a hospital that specializes in the diagnosis and treatment of strokes, as long as it is not too far away. The patient is then thoroughly examined to find out the cause of the symptoms. That includes CT or MRI scans.
After the paramedics have provided first aid, the patient will be taken to a hospital that specializes in the diagnosis and treatment of strokes, as long as it is not too far away. The patient is then thoroughly examined to find out the cause of the symptoms. That includes CT or MRI scans.
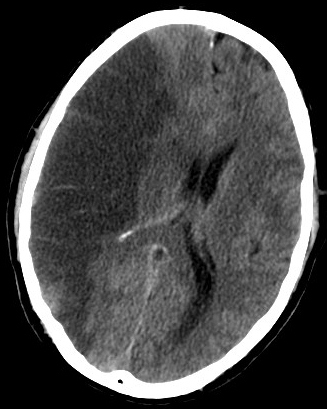 |
| Stroke. Infarction of brain. CT scan. |
Prevention
Whether particular preventive measures against a stroke are worthwhile depends on any other conditions and risk factors that someone might have.
Doctors will usually suggest preventive measures after precisely examining people who have already had a transient ischemic attack or even a stroke.
People with high blood pressure can reduce their risk of a stroke by taking blood-pressure lowering medication. If somebody has an increased risk of blood clots, for example due to long term atrial fibrillation, anticoagulant (blood-thinning) medication can be an option.
Fitness training as part of rehabilitation after a stroke can increase physical fitness and improve mobility.
A stroke damages the brain because it disrupts the blood flow. Most people survive a stroke. But they may be left with paralysis in certain parts of the body or problems with abilities, for example speech. Psychological problems such as depression are also possible.
It is often very important to regain mobility, strength and speech after a stroke, as well as keeping any restrictions of independence to a minimum. It is also important to restore emotional stability.
At first glance it may seem less important to remain physically fit. But not only your fitness suffers if you can not move around so well: People who are not that fit also have more difficulty doing exercises that promote recovery and maintain independence. A vicious circle can then begin: If you are less fit, you are not as active, and that means that you become even more unfit.
Fitness is important for other things too though, for example a healthy heart. Fitness can also play a role in preventing another stroke or lowering the risk of other problems such as high blood pressure (hypertension).
The following three types of training were analyzed in the studies:
Acceptance for these fitness programs was very high. The participants in the studies attended an average of 65 to 100 % of the training sessions. The cardiovascular exercises had a number of benefits. There were signs that the heart and lungs became fitter and the participants' mobility improved. For example, they were able to walk faster and had more stamina. That reduced the physical restrictions resulting from the stroke. Programs that combined cardiovascular and weight training also improved mobility. Weight training alone had no influence on mobility. There has not been enough research to say what the other effects of weight training might be.
It is possible that fitness training could also have side effects - for example muscle injuries, falls or heart problems. However, the programs assessed in the studies seemed to be very safe. No falls, broken bones or injuries were observed during the fitness training programs and there was no increase in the number of heart attacks.
Regaining strength and fitness after a stroke can require a lot of effort and motivation. But even minor improvements can mean real progress.
Depression after a stroke
Some people develop depression after a stroke. It is important that it is diagnosed and treated. Good medical treatment and care along with support from family and friends are crucial.
Grief and sadness are normal after a stroke. But some people might also become depressed and need professional treatment. This is actually quite common, and affects around a third of all stroke patients. Women may have a slightly higher risk of becoming depressed following a stroke.
Depression is not always noticed and treated properly after a stroke. The condition is also called "post-stroke depression" (PSD).
Depression normally occurs within the first few weeks after a stroke. During that time people have to come to terms with having experienced this life-threatening situation and have to recover physically. Some people will have to get used to disabilities and how they affect their daily lives, and communication with friends and family can also change. Not everyone manages that straight away, and sometimes that is the very cause of depression for some people.
Depression is more common after a major stroke than after a mild one, and is also more likely in people who have already suffered from depression. The severity of a person's depression often depends on how physically or mentally restricted they are in daily life. Studies have shown that a person's social environment, living arrangements and the support they get can also influence the likelihood of developing depression. Good care and social support can help reduce the risk of depression developing following a stroke.
A number of other possible influences have not yet been researched properly. For example, it is not clear how much factors like difficulty speaking and understanding (aphasia), signs of confusion or dementia influence the development of depression. Sometimes post-stroke depression goes away after a while without treatment. Most people do however require treatment to get over the illness.
Depression after a stroke is diagnosed in the same way as "normal" depression. The symptoms are:
Sometimes people who are depressed are over-emotional. They might have less control over how they express their emotions after a stroke, and find that they suddenly start crying – or laughing – in inappropriate situations. They may also generally have more mood swings and react very emotionally.
People who are caring for somebody who has had a stroke can also develop depression, especially if the care gets too much for them. It is of course more difficult for people with depression to give somebody who has had a stroke as much help as they usually would. The person who had the stroke may then also find it harder to control their own emotions. So looking after the carers is not only important for them and other family members, but also for the person who had the stroke. Giving carers enough support is part of providing good care to someone who has had a stroke.
The medication does not have an immediate effect. However, symptoms usually begin to improve within the first six to eight weeks. Some people also find that the symptoms of their depression go away without taking antidepressants. The general rule is: The more severe a depression, the greater the benefit of medication. But there is no guarantee of success. Depression can remain despite taking medication, or it can return.
Antidepressants can also have side effects, including drowsiness, cramps, bleeding and digestion problems. There is however not enough research to say how often such side effects are experienced by people who have had a stroke. Because walking can be difficult or only possible with a walking aid after a stroke, it is especially important to pay attention to side effects that influence coordination. Dizziness and drowsiness can increase the risk of falling, for example. There is not enough research on the effects of antidepressants for people with special problems such as trouble speaking or understanding.
Antidepressants can also interact with other medication and affect how it works. For those and other reasons, doctors carefully monitor people who take medication to treat post-stroke depression. It could be necessary for them to stop taking or change the medication.
Medication and psychological therapy are not the only options for preventing and treating depression. Everyday support from relatives or professional carers can play an important role in the recovery process and in coping with disabilities. The more support people receive, the more successful their rehabilitation after a stroke is likely to be. In turn, good physical recovery can have a positive effect on mental health.
Simple words of encouragement and advice usually do not help to motivate people who are depressed. It takes a lot of sensitivity and patience to cope with their condition. What is more, people with depression can be prone to mood swings. Depression can also take many different forms. For example, older people with depression complain more often about pain than younger people.
There are a number of support centers and self-help groups that provide people who have depression and those close to them with advice about various health care, financial or psychosocial matters. For example, many cities and local authorities offer special information services on nursing care, free of charge. Family members can also take part in care courses to learn basic care techniques. Looking after a family member who has had a stroke can be a major challenge, but there is a lot of help available.
Sources
Doctors will usually suggest preventive measures after precisely examining people who have already had a transient ischemic attack or even a stroke.
People with high blood pressure can reduce their risk of a stroke by taking blood-pressure lowering medication. If somebody has an increased risk of blood clots, for example due to long term atrial fibrillation, anticoagulant (blood-thinning) medication can be an option.
Treatment
Acute treatment aims to save a person's life and minimize the damage of the stroke as much as possible. The type of treatment mainly depends on whether the stroke was caused by a blood clot or a hemorrhage.
If it was caused by a blood clot, the doctors generally try to dissolve it as quickly as possible using medication or a catheter. Brain hemorrhages have to be stopped quickly, where necessary by operating.
Further treatment and observation then depends on the severity of the stroke, the type of symptoms afterwards, and the results of further examinations.
The most frequently used antiplatelets are medications that contain the active ingredient acetylsalicylic acid (ASA). There is a lot of experience with this ingredient and it has been proven to be able to lower the risk of complications following a stroke. Clopidogrel (Plavix) is another antiplatelet.
Antiplatelets can also have side effects - especially bleeding. Light bleeding, as with nose bleeds, is usually not a problem. But heavy gastrointestinal bleeding (bleeding in the stomach and bowel) is also possible, and urgent medical treatment is needed if that happens.
Another antiplatelet that can be taken to prevent cardiovascular diseases after a stroke has been available for a while now: Dipyridamole (Persantine). The drug is only approved in Germany in combination with ASA. The trade name of the combination drug is Aggrenox.
The Institute for Quality and Efficiency in Health Care (IQWiG, Germany) has analysed the advantages and disadvantages of this medication:
A combination of dipyridamole and ASA leads more frequently to side effects and complications than clopidogrel or ASA taken alone. There is no proof that the combination has advantages over just taking clopidogrel or ASA on their own.
If it was caused by a blood clot, the doctors generally try to dissolve it as quickly as possible using medication or a catheter. Brain hemorrhages have to be stopped quickly, where necessary by operating.
Further treatment and observation then depends on the severity of the stroke, the type of symptoms afterwards, and the results of further examinations.
The most frequently used antiplatelets are medications that contain the active ingredient acetylsalicylic acid (ASA). There is a lot of experience with this ingredient and it has been proven to be able to lower the risk of complications following a stroke. Clopidogrel (Plavix) is another antiplatelet.
Antiplatelets can also have side effects - especially bleeding. Light bleeding, as with nose bleeds, is usually not a problem. But heavy gastrointestinal bleeding (bleeding in the stomach and bowel) is also possible, and urgent medical treatment is needed if that happens.
Another antiplatelet that can be taken to prevent cardiovascular diseases after a stroke has been available for a while now: Dipyridamole (Persantine). The drug is only approved in Germany in combination with ASA. The trade name of the combination drug is Aggrenox.
The Institute for Quality and Efficiency in Health Care (IQWiG, Germany) has analysed the advantages and disadvantages of this medication:
A combination of dipyridamole and ASA leads more frequently to side effects and complications than clopidogrel or ASA taken alone. There is no proof that the combination has advantages over just taking clopidogrel or ASA on their own.
Rehabilitation
It is often very important for people to regain their mobility, muscle strength, speech, and independence after having a stroke. It is also important to restore emotional balance.
There are various rehabilitation programs with different contents. Different therapists prefer different treatments, and there are also differences from country to country.
The main elements of rehabilitation include speech therapy, physiotherapy and fitness training to try and minimize any physical disabilities and learn to deal with them. Rehabilitation also includes occupational therapy, where patients learn how they can go about their daily lives as independently as possible despite any restrictions.
There are various rehabilitation programs with different contents. Different therapists prefer different treatments, and there are also differences from country to country.
The main elements of rehabilitation include speech therapy, physiotherapy and fitness training to try and minimize any physical disabilities and learn to deal with them. Rehabilitation also includes occupational therapy, where patients learn how they can go about their daily lives as independently as possible despite any restrictions.
Fitness training as part of rehabilitation after a stroke can increase physical fitness and improve mobility.
A stroke damages the brain because it disrupts the blood flow. Most people survive a stroke. But they may be left with paralysis in certain parts of the body or problems with abilities, for example speech. Psychological problems such as depression are also possible.
It is often very important to regain mobility, strength and speech after a stroke, as well as keeping any restrictions of independence to a minimum. It is also important to restore emotional stability.
At first glance it may seem less important to remain physically fit. But not only your fitness suffers if you can not move around so well: People who are not that fit also have more difficulty doing exercises that promote recovery and maintain independence. A vicious circle can then begin: If you are less fit, you are not as active, and that means that you become even more unfit.
Fitness is important for other things too though, for example a healthy heart. Fitness can also play a role in preventing another stroke or lowering the risk of other problems such as high blood pressure (hypertension).
Research on fitness training after a stroke
Researchers from the Cochrane Collaboration – an international network of researchers – looked for studies which evaluated the benefits of fitness training after a stroke. They looked for randomized controlled studies because they provide the best information for assessing how medical treatments affect health. The researchers found 45 studies with a total of almost 2,200 men and women who had had a stroke. The average age was 64.The following three types of training were analyzed in the studies:
- Cardiovascular programs for healthy heart and lungs (22 studies)
- Weight training (8 studies)
- Programs which combined cardiovascular and weight training (15 studies)
Acceptance for these fitness programs was very high. The participants in the studies attended an average of 65 to 100 % of the training sessions. The cardiovascular exercises had a number of benefits. There were signs that the heart and lungs became fitter and the participants' mobility improved. For example, they were able to walk faster and had more stamina. That reduced the physical restrictions resulting from the stroke. Programs that combined cardiovascular and weight training also improved mobility. Weight training alone had no influence on mobility. There has not been enough research to say what the other effects of weight training might be.
It is possible that fitness training could also have side effects - for example muscle injuries, falls or heart problems. However, the programs assessed in the studies seemed to be very safe. No falls, broken bones or injuries were observed during the fitness training programs and there was no increase in the number of heart attacks.
Regaining strength and fitness after a stroke can require a lot of effort and motivation. But even minor improvements can mean real progress.
Everyday life
It is normal to feel sad and depressed after a stroke. Depending on the severity of the stroke, it can considerably restrict a patient's life.
People who lived independently before and are then dependent on others for help first have to learn to come to terms with the effects of the stroke, both the physical consequences as well as in practical everyday situations.
That is why therapy can help people to regain some of their independence after a stroke. Over time, most patients and their families manage to adapt their lives to the changes.
However, as a result of a stroke some people develop depression that requires treatment from trained professionals. If the depression lasts for a long time it can affect a patient's overall health. These kinds of depression often go unnoticed, or sadness and feeling down is considered to be a normal reaction and no steps are taken to treat it.
It is not always easy to differentiate between deep sadness and depression after a stroke. It is important that patients and their families receive the support that they need to prevent depression, or are offered help if depression has already set in.
People who lived independently before and are then dependent on others for help first have to learn to come to terms with the effects of the stroke, both the physical consequences as well as in practical everyday situations.
That is why therapy can help people to regain some of their independence after a stroke. Over time, most patients and their families manage to adapt their lives to the changes.
However, as a result of a stroke some people develop depression that requires treatment from trained professionals. If the depression lasts for a long time it can affect a patient's overall health. These kinds of depression often go unnoticed, or sadness and feeling down is considered to be a normal reaction and no steps are taken to treat it.
It is not always easy to differentiate between deep sadness and depression after a stroke. It is important that patients and their families receive the support that they need to prevent depression, or are offered help if depression has already set in.
Depression after a stroke
Some people develop depression after a stroke. It is important that it is diagnosed and treated. Good medical treatment and care along with support from family and friends are crucial.
Grief and sadness are normal after a stroke. But some people might also become depressed and need professional treatment. This is actually quite common, and affects around a third of all stroke patients. Women may have a slightly higher risk of becoming depressed following a stroke.
Depression is not always noticed and treated properly after a stroke. The condition is also called "post-stroke depression" (PSD).
Why can depression occur following a stroke?
It is not exactly clear whether depression after a stroke has mainly physical or mental causes. After all, a stroke damages the brain and those damages can also affect people's emotions. But depression can also be a reaction to physical and mental limitations and the sudden loss of independence. That is called "reactive depression".Depression normally occurs within the first few weeks after a stroke. During that time people have to come to terms with having experienced this life-threatening situation and have to recover physically. Some people will have to get used to disabilities and how they affect their daily lives, and communication with friends and family can also change. Not everyone manages that straight away, and sometimes that is the very cause of depression for some people.
Depression is more common after a major stroke than after a mild one, and is also more likely in people who have already suffered from depression. The severity of a person's depression often depends on how physically or mentally restricted they are in daily life. Studies have shown that a person's social environment, living arrangements and the support they get can also influence the likelihood of developing depression. Good care and social support can help reduce the risk of depression developing following a stroke.
A number of other possible influences have not yet been researched properly. For example, it is not clear how much factors like difficulty speaking and understanding (aphasia), signs of confusion or dementia influence the development of depression. Sometimes post-stroke depression goes away after a while without treatment. Most people do however require treatment to get over the illness.
How can you tell if someone is depressed after a stroke?
It is important to remember that there is a difference between depression and the feelings of sadness caused by a stroke. Strokes often lead to paralysis on one side of the body. That can seriously affect a person's ability to move or lead an independent life. Everyday activities like eating and washing may become difficult without the help of others. On top of this, a person may have little or no feeling in the paralysed side of their body. Problems with speech or understanding could be a further burden. Not being able to communicate properly can be very depressing. Some people may just appear depressed to others because they are unable to express their emotions as easily as they could before their stroke. Detecting post-stroke depression (PSD) is therefore not so easy.Depression after a stroke is diagnosed in the same way as "normal" depression. The symptoms are:
- Deep sadness
- Loss of interest
- Listlessness
- Poor concentration
- Low self-esteem
- Sleep disorders
Sometimes people who are depressed are over-emotional. They might have less control over how they express their emotions after a stroke, and find that they suddenly start crying – or laughing – in inappropriate situations. They may also generally have more mood swings and react very emotionally.
How are patients and those close to them affected by depression?
Being depressed can slow down recovery after a stroke. Whether or not stroke-related disabilities improve depends on a number of factors, including how actively a person participates in their therapy. For example, certain physical exercises can help to improve movement on the paralysed side of the body. It often takes a long time to recover from a stroke, and can require a lot of patience and motivation. People with depression find it more difficult to motivate themselves and may not be able to work as hard to restore their health as people who are not depressed. As a result, it could take them longer to recover, or their physical and mental abilities may even get worse.People who are caring for somebody who has had a stroke can also develop depression, especially if the care gets too much for them. It is of course more difficult for people with depression to give somebody who has had a stroke as much help as they usually would. The person who had the stroke may then also find it harder to control their own emotions. So looking after the carers is not only important for them and other family members, but also for the person who had the stroke. Giving carers enough support is part of providing good care to someone who has had a stroke.
What treatment options are available?
Depression is often treated with medication (antidepressants) and / or psychological methods such as counseling or psychotherapy. The treatment options include support, learning about your thought patterns, stress management techniques and relaxation strategies. Some people also use complementary therapies, like massage or herbal products with ingredients like St John's wort (hypericum).Antidepressants
Studies show that antidepressants can help people with post-stroke depression. They may also have a positive effect on physical recovery. The following two groups of antidepressants have been studied the most: Selective serotonin reuptake inhibitors (SSRI) and tricyclic antidepressants. They are among the most frequently prescribed drugs for treating depression.The medication does not have an immediate effect. However, symptoms usually begin to improve within the first six to eight weeks. Some people also find that the symptoms of their depression go away without taking antidepressants. The general rule is: The more severe a depression, the greater the benefit of medication. But there is no guarantee of success. Depression can remain despite taking medication, or it can return.
Antidepressants can also have side effects, including drowsiness, cramps, bleeding and digestion problems. There is however not enough research to say how often such side effects are experienced by people who have had a stroke. Because walking can be difficult or only possible with a walking aid after a stroke, it is especially important to pay attention to side effects that influence coordination. Dizziness and drowsiness can increase the risk of falling, for example. There is not enough research on the effects of antidepressants for people with special problems such as trouble speaking or understanding.
Antidepressants can also interact with other medication and affect how it works. For those and other reasons, doctors carefully monitor people who take medication to treat post-stroke depression. It could be necessary for them to stop taking or change the medication.
Psychological and psychotherapeutic support
Expert support is a key element in treating depression and might also be advisable for people who have had a stroke. Psychiatrists, psychologists and trained counselors in hospitals or rehabilitation clinics can help people to come to terms with their condition and the changes to their lives. There are however as yet no conclusive studies on this topic. Help can also be found at psychosocial centers.Medication and psychological therapy are not the only options for preventing and treating depression. Everyday support from relatives or professional carers can play an important role in the recovery process and in coping with disabilities. The more support people receive, the more successful their rehabilitation after a stroke is likely to be. In turn, good physical recovery can have a positive effect on mental health.
How can you help people with post-stroke depression?
People recover better from a stroke if everybody involved gives their full support. Research has shown that people cope more successfully in the long term if treatment is very well organised, and nurses, doctors, physiotherapists and people close to them actively participate in their care. Occupational therapy in particular can help to regain certain physical abilities. This involves working on daily activities like washing, getting dressed and doing things around the house. Successful rehabilitation therapy requires a lot of motivation, but it can make an important difference to people's lives after a stroke.Simple words of encouragement and advice usually do not help to motivate people who are depressed. It takes a lot of sensitivity and patience to cope with their condition. What is more, people with depression can be prone to mood swings. Depression can also take many different forms. For example, older people with depression complain more often about pain than younger people.
There are a number of support centers and self-help groups that provide people who have depression and those close to them with advice about various health care, financial or psychosocial matters. For example, many cities and local authorities offer special information services on nursing care, free of charge. Family members can also take part in care courses to learn basic care techniques. Looking after a family member who has had a stroke can be a major challenge, but there is a lot of help available.
Sources
