Pittsburgh: In a landmark trial conducted at Children’s Hospital of Pittsburgh of UPMC and the University of Pittsburgh School of Medicine,
researchers have demonstrated that when treating children between 6 and
23 months of age with antibiotics for ear infections, a shortened
course has worse clinical outcomes without reducing the risk of
antibiotic resistance or adverse events. The results of the trial are published today in the New England Journal of Medicine and highlighted by an accompanying commentary.
Acute
otitis media is a bacterial infection of the middle ear behind the ear
drum which causes it to become painfully inflamed. Three out of four
children experience this infection within their first year.
Consequently, it is the most common reason why children are prescribed
an antibiotic.
“Given significant concerns regarding overuse of
antibiotics and increased antibiotic resistance, we conducted this trial
to see if reducing the duration of antibiotic treatment would be
equally effective along with decreased antibiotic resistance and fewer
adverse reactions,” said Alejandro Hoberman, M.D., chief, Division of
General Academic Pediatrics at Children’s, and the Jack L. Paradise
Endowed Professor of Pediatric Research at Pitt’s School of Medicine.
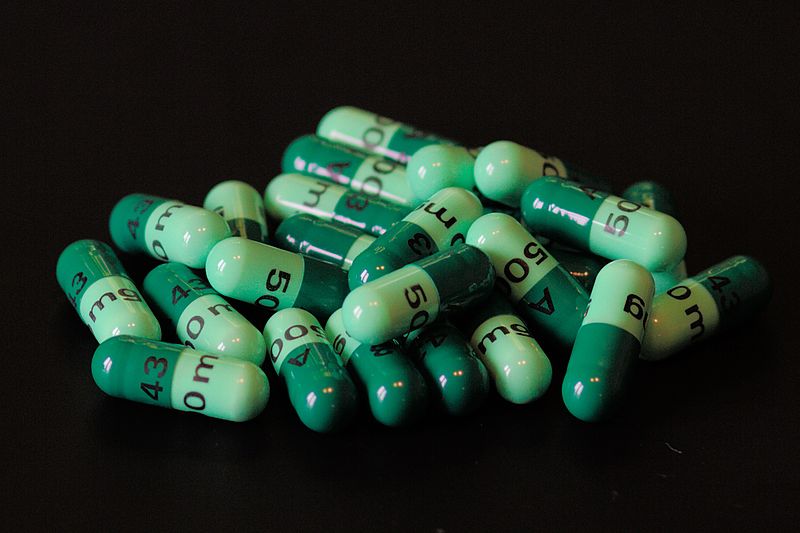
In
the current trial, 520 children with acute otitis media were randomly
assigned to either a standard 10-day regimen of the antibiotic
amoxicillin-clavulanate or a shortened 5-day treatment followed by five
days of placebo. Neither the study participants nor the physicians knew
which group the participant was assigned to.
Children were
followed starting in October through the rest of the annual
respiratory-infection season, and had a final visit during the following
September.
They found that the risk of treatment failure in
the 5-day group (34 percent) was more than twice as much the risk in the
10-day group (16 percent). The results were significant when
considering the trial design which was set up to find out whether the
5-day treatment would be as good as the 10-day regimen, Dr. Hoberman
said. Instead, the results clearly showed that not only was their
initial assumption proven wrong, but the 10-day treatment was far more
effective.
When they tested the presence of antibiotic-resistant
bacteria through nasopharyngeal (back of the nose) swabs, there was no
decrease in the 5-day group as might have been expected with a shorter
duration of antibiotics. Also, reduced-duration antibiotics did not
decrease the risk of frequent adverse events like diarrhea or diaper
rash.
When testing the risk of a recurrent infection, they found
that it was higher when children were exposed to three or more children
for 10 or more hours per week, such as in a day care setting, or if the
initial infection occurred in both ears as opposed to just one ear.
Importantly,
the study also showed for the first time that almost one in two
children in whom residual fluid was observed in the middle ear after
treatment had a recurring infection, a significantly higher percentage
when compared to children without any residual fluid in the middle ear.
The
marked superiority of the 10-day regimen over the 5-day regimen led the
independent safety monitoring board overseeing the trial to conclude it
prematurely as the primary end point was achieved.
“The results
of this study clearly show that for treating ear infections in children
between 9 and 23 months of age, a 5-day course of antibiotic offers no
benefit in terms of adverse events or antibiotic resistance. Though we
should be rightly concerned about the emergence of resistance overall
for this condition, the benefits of the 10-day regimen greatly outweigh
the risks,” said Dr. Hoberman.
The study was supported by a contract (HHSN272201000047C) from the National Institute of Allergy and Infectious Diseases and by University of Pittsburgh Clinical and Translational Science Awards
(UL1RR024153 and UL1TR000005) from the National Center for Research
Resources, now at the National Center for Advancing Translational
Sciences, National Institutes of Health.
Other authors include
Jack L. Paradise, M.D., Howard E. Rockette, Ph.D., Diana H. Kearney,
R.N., C.C.R.C., Sonika Bhatnagar, M.D., M.P.H., Timothy R. Shope, M.D.,
M.P.H., Judith M. Martin, M.D., Marcia Kurs-Lasky, M.S., Susan J.
Copelli, B.S., D. Kathleen Colborn, B.S., Stan L. Block, M.D., John J.
Labella, M.D., Thomas G. Lynch, M.D., Norman L. Cohen, M.D., MaryAnn
Haralam, C.R.N.P., Marcia A. Pope, R.N., Jennifer P. Nagg, R.N., Michael
D. Green, M.D., M.P.H., and Nader Shaikh, M.D., M.P.H., all from
Children’s Hospital of Pittsburgh of UPMC and the University of
Pittsburgh.