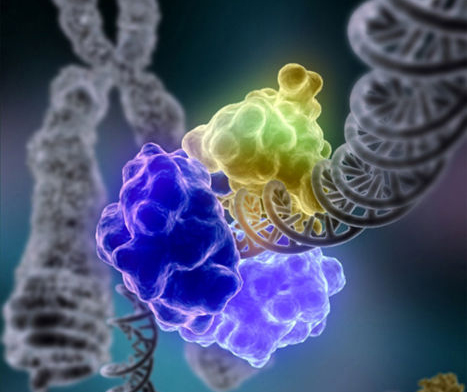
Pittsburgh: Research by scientists at the University of Pittsburgh Cancer Institute
(UPCI) has revealed how cancer cells hijack DNA repair pathways to
prevent telomeres, the endcaps of chromosomes, from shortening, thus
allowing the tumor to spread. The findings are published today in the
journal Cell Reports. The moment a cell is formed, a countdown clock starts ticking that
determines how long the cell can live. The clock is the telomere, a
series of repeating DNA letters at the ends of each chromosome in the
cell.
However, cancer cells cleverly hijack this telomere clock,
resetting it and lengthening the telomere every time it shortens. This
leads the cell into thinking that it is still young and can divide,
spreading the tumor.
Most cancers do this by increasing the activity of an enzyme called
telomerase which lengthens telomeres. But approximately 15 percent of
cancers use a different mechanism for resetting the clock, called
alternative lengthening of telomeres (ALT).
Growing evidence also suggests that tumors that activate the ALT
pathway are aggressive and more resistant to treatment. Although ALT was
identified close to two decades ago, identifying how this mechanism
works has proved elusive.
“Identifying the parts that the cancer cell tweaks to reset the
countdown timer could provide targets for developing new cancer drugs or
making existing ones more effective,” said senior author Roderick
O’Sullivan, Ph.D., assistant professor of pharmacology and chemical
biology at Pitt’s School of Medicine and a member of UPCI.
O’Sullivan and his team tackled this problem by using a recently
developed technique called proximity dependent biotinylation (BioID),
which allowed them to quickly identify proteins that were physically
close to, and hence potentially associated with, telomere lengthening in
cancer cells.
When comparing cancer cells in which either telomerase or ALT were
active, the BioID technique identified 139 proteins that were unique to
ALT-activated cells. As the research team took a closer look, one
enzyme, DNA polymerase η (Polη), took them by surprise.
“We expected to see DNA repair proteins, but seeing Polη was really
unexpected as it was known to be activated only in cells that were
damaged by UV light, which we did not use in our experiments. Its role
in the ALT pathway is completely independent of how we think of it
normally,” said O’Sullivan. Knowing the molecular players in the ALT
pathway opens up a whole new area of research and many potential drug
targets, according to O’Sullivan.
Laura Garcia-Exposito, Ph.D., a postdoctoral fellow in O’Sullivan’s
lab, and Elodie Bournique, a graduate student in the laboratory of Dr.
Jean-Sébastien Hoffmann at the Cancer Research Center of Toulouse,
France, are the co-first authors of the study.
Other study authors include Arindam Bose, Ph.D., Simon C. Watkins,
Ph.D., Patricia Opresko, Ph.D., Callen Wallace and Justin L. Roncaioli,
all of the University of Pittsburgh; Valérie Bergoglio, Ph.D., and
Jean-Sébastien Hoffmann Ph.D., of the Cancer Research Center at the
University of Toulouse; Sufang Zhang, Ph.D., and Marietta Lee Ph.D., of
New York Medical College.
This research was funded by grants from the Competitive Medical
Research Fund and Stimulating Pittsburgh Research in Geroscience at the
University of Pittsburgh, National Institutes of Health grants ES022944, P30CA047904, 1S10OD019973-O1; and INCa-PLBIO 2016, ANR PRC 2016, Labex Toucan, and La Ligue contre le Cancer.