Author: Dr Brent Yanke Urologist West Orange New Jersey 2008-07-28
Hematuria: Blood in the Urine
KIDNEY ANATOMY AND FUNCTION
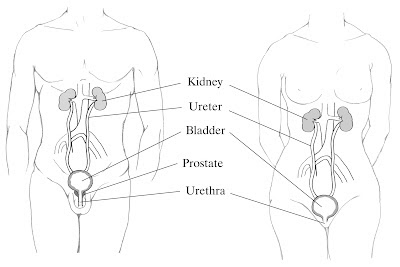
The
kidneys are organs responsible for cleansing the blood of waste. Many
byproducts of metabolic processes in the body build up in the
bloodstream. A microscopic tubular system within the kidney filters the
blood and removes these byproducts before they can accumulate to
dangerous levels. Once blood enters the kidney, it is transported to a
collection of small capillary vessels, called the glomerulus. As the
blood passes through the glomerulus, the filtrated waste shifts to
Bowman’s capsule, a pouch that surrounds the glomerulus and starts the
tubular system. Kidney tissue is separated into two layers: the outer
cortex and the inner medulla. Once the filtered waste passes through
these layers, it reaches the renal papillae which project into the renal
pelvis, an open space in the core of the kidney, where the urine
collects. The urine then drains from the renal pelvis into the ureter
and finally into the bladder. The kidneys and ureters comprise the upper
urinary tract, while the bladder and urethra comprise the lower urinary
tract (Figure 1).
Figure 1. Anatomic Representation of the Male (Left) and Female (Right) Urinary Tract
Courtesy of National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
WHAT IS HEMATURIA AND HOW IS IT CLASSIFIED?
Hematuria is the presence of blood in the urine. Studies have found it in 2.5% to 21% of the general population.1 When the blood is visible to the patient, it is referred to as gross hematuria. More often, blood is found on routine testing and is visible only by microscopic analysis; this is termed microscopic hematuria.
The American Urological Association defines microscopic hematuria as
the presence of three or more red blood cells per high-power field on
microscopic evaluation from two out of three urine specimens.2
As
discussed below, the presence of microscopic hematuria can prompt
various degrees of evaluation based on the clinical situation, ranging
from complete examination to none at all. However, gross hematuria
should always lead to a full urologic work-up due the higher risk of
malignancy (cancer). Several large studies have shown much higher rates
of malignancy with gross hematuria (18% to 25%) compared with
microscopic hematuria (3% to 5%).3,4
ARE THERE SYMPTOMS ASSOCIATED WITH HEMATURIA?
The
majority of patients who come to the doctor with hematuria have no
accompanying symptoms. However, certain associated symptoms can suggest a
particular medical condition.
Pain is frequently found with
microscopic and gross hematuria. Both pain and hematuria can be caused
by a common underlying source, or the pain can be a direct result of the
hematuria itself. Often the location and nature of the pain can give a
clue to the cause. Sharp flank or lower abdominal pain suggests that the
ureter is blocked, called ureteral obstruction. This may be caused by a
passing stone with resulting pain and hematuria following ureteral
trauma. Likewise, clots formed from bleeding in the upper urinary tract
can cause similar pain when traveling through the ureter. These clots
tend to be thin and wormlike, while clots formed in the bladder and
prostatic urethra are more likely to be larger and appear as nonspecific
clumps.5 Pain associated with urination may be more
indicative of a bladder infection, particularly when urinary frequency
and urgency are present as well. While these infections tend to cause
microscopic hematuria, gross hematuria is also common.
In men
with an enlarged prostate, called benign prostatic hypertrophy (BPH),
hematuria can be present with symptoms of bladder obstruction. These
patients can have slow urinary stream, difficulty initiating urination,
and urinary frequency and urgency at night. While the hematuria is
generally painless, the formation of clots in the bladder and prostate
can lead to complete obstruction and an inability to urinate with
resulting discomfort.
It is
important for any patient with urinary symptoms and hematuria to be
evaluated for a bladder tumor. These tumors can cause urinary urgency
and frequency and may mimic the above benign conditions.
THE CAUSES OF HEMATURIA
The
initial assessment of hematuria centers on establishing the potential
sources. Namely, it must be determined whether the cause is of
glomerular origin or nonglomerular origin. Microscopic urinalysis
provides essential information in differentiating these.
The urine specimen of patients with glomerular disease often exhibits one or more of the following:
- Proteinuria – This is the presence of protein in the urine. Normally, the glomeruli prevent a significant amount of protein from entering the forming urine. Urine protein levels higher than 1,000 mg for a 24-hour period are highly suggest glomerular disease. Even considerable amounts of gross hematuria from nonglomerular causes do not raise protein concentrations to this level.5
- Red blood cell casts – Casts are cells seen clumped together in the urinalysis. The source of casts is from the glomeruli of the kidney. Blood cells are normally prevented from passing through the glomeruli into the renal tubular system. However, when glomerular damage is present, blood cells can pass into the tubules where they cluster together to form casts. Although casts are generally not seen in nonglomerular hematuria, the absence of casts does not exclude glomerular sources as up to 20% of these patients can have hematuria without casts.6
- Red blood cell shape – Normal red blood cells are round with similar size and shape. This is typical of nonglomerular bleeding. However, bleeding of glomerular origin leads to irregularly shaped red blood cells of varying size.7-9
CAUSES OF GLOMERULAR HEMATURIA
Many
diseases can affect the renal glomerulus leading to hematuria. Common
causes are listed below. Although learning that blood is present in the
urine can be an upsetting experience, a majority of the glomerular
causes actually are rather harmless and have no major long-term
consequences.
IgA Nephropathy (Berger’s Disease)
- The most common diagnosis in patents with glomerular hematuria representing approximately 30% of all cases.6
- Hematuria can be either gross or microscopic.
- More frequently diagnosed in younger patients and in men.
- Gross hematuria is more common in children, but hematuria is more likely to be microscopic with advancing age.10
- The disease can present as hematuria after an upper respiratory infection particularly in younger patients.
- It is diagnosed by renal biopsy.
- Most of these patients will encounter few, if any, long-term health concerns. However, in 5% to 25% of patients, the disease will progress.11 These patients will develop various degrees of renal failure along with worsening proteinuria and elevated blood pressure.
Familial Nephritis (Alport’s Syndrome)
- This accounts for roughly 10% of glomerular hematuria cases.6
- There is invariably gross hematuria.
- It is hereditary with multiple genetic mutations present.
- A strong family history of renal failure is present, often with multiple family members affected.
- Other associated symptoms include deafness and eye abnormalities.
Other Glomerulonephritis (GN) Syndromes
- Membranous GN – Patients undergo the following three clinical courses in roughly equal proportions: Resolution of the disease, continued disease but with stable kidney function, and renal failure.
- Focal Segmental Glomerulosclerosis – Approximately half progress to renal failure.
- Systemic Lupus Erythematosus – This is an autoimmune disease that predominantly occurs in women. Almost any part of the body can be affected by the disease and its severity is extremely variable. The kidneys are involved in a majority of patients, but most have no symptoms and few progress to renal failure. Gross or microscopic hematuria can be seen and occasionally can be the first and only symptom.
- Poststreptococcal GN – Generally temporary with little risk of permanent injury, this can be seen in young patients who have had a recent streptococcal upper respiratory infection.
CAUSES OF NONGLOMERULAR HEMATURIA
Nonglomerular
causes of hematuria can be due to a large array of processes throughout
the upper and lower urinary tract. Diseases such as cancer, infection,
and stones all need to be considered when evaluating for urological
sources of hematuria. The more notable causes are listed by organ below.
Kidney
Kidney Cancer
Historically,
the common presentation of kidney cancer involved one or more of the
triad of gross hematuria, flank pain, and a flank mass. However,
hematuria rarely is seen as an early symptom in modern times. This is
due to the widespread use of radiologic imaging, which has allowed these
cancers to be found much earlier before hematuria has developed.
However, some renal cancers may still be diagnosed at an advanced stage.
Gross hematuria may be present when the tumor invades into the renal
pelvis and urinary collecting system, while microscopic hematuria may
result from invasion of the cancer into normal kidney tissue.
Urethelial Cancer of the Renal Pelvis
Urothelial
cancer of the renal pelvis arises from the cells that line the renal
pelvis of the kidney where urine first collects. As is seen with renal
cancers, hematuria may be gross or microscopic.
Stones and Hypercalciuria
Stones
of any size can cause hematuria by traumatizing the urothelial lining
within the kidney (Figure 2). When the stones remain in the kidney, the
hematuria may not be associated with pain. Hematuria has also been
linked to hypercalciuria (elevated levels of calcium in the urine).12
These patients have a strong family history of stone disease and
treatment with thiazide diuretics generally leads to resolution of the
hematuria.
Figure 2. Endoscopic View of Bleeding Caused by a Renal Stone
Pyelonephritis
Infection
of the kidney, termed pyelonephritis, can often cause hematuria. This
should be suspected when the hematuria occurs in conjunction with back
pain, fevers, and chills. Treatment of the infection with antibiotics
will halt the hematuria.
Hereditary Renal Disease
- Cystic Disease – Adult polycystic kidney disease (APKD) and medullary sponge kidney (MSK) are inherited disorders where cysts, or pouches filled with fluid, form within the kidney. APKD invariably leads to renal failure while MSK does not. Hematuria is due to cysts that bleed into the collecting system.
- Papillary Necrosis – Papillae within the kidney die and shed into the renal pelvis and ureter causing hematuria and pain from obstruction. This can be seen in sickle cell disease, a hereditary disease seen in African-Americans that causes the body’s red blood cells to be abnormal. It has also been associated with diabetes and ingestion of Phenacetin, an analgesic medication not commonly used today.
Vascular Disease
- Arteriovenous Fistulas – These are abnormal collections of blood vessels that frequently bleed and can be a source of persistent painless hematuria. Although more common in the kidney, they can occur at any location along the urinary tract.
- Renal Artery and Vein Thrombosis – A thrombosis is a clot that forms within a blood vessel. When this occurs in the renal artery, a portion of the kidney may infarct (die) leading to pain and hematuria. A thrombosis in the renal vein reduces the ability of blood to drain from the kidney.
Ureter
Stones
As
stones pass from the kidney into the ureter, they will frequently cause
pain along with hematuria. The hematuria may be microscopic or gross
and is a result of trauma to the urothelial lining of the ureter as the
stone descends. There may also be urinary symptoms such as frequency and
urgency once the stone reaches the last part of the ureter and passes
into the bladder.
Ureteral Cancer
Tumors
of the ureter may present with hematuria as well as pain and renal
failure due to obstruction of the ureter. These tumors can present with a
jet of blood entering the bladder from the involved ureter.
Bladder
Stones
Aside
from stones that have passed into the bladder from the upper urinary
tract, hematuria can be caused by stones that have formed within the
bladder. This is typically seen in patients with benign prostatic
hypertrophy (BPH) where an enlarged prostate obstructs the bladder. As a
result, the bladder may be unable to empty urine completely, and
crystals within the urine form stones. It is common to have multiple
stones in this setting, with some growing larger than a golf ball.
Bladder Cancer
Tumors
of the bladder almost always present with hematuria. Larger tumors may
bleed profusely, causing the urine to turn deep red and resulting in
clot formation (Figure 3). The clots may be rather large and fill the
bladder. When this occurs, the clots may obstruct the bladder, and the
patient may have pain and an inability to urinate.
Figure 3. Endoscopic View of Bleeding from a Bladder Tumor
Cystitis
Common
causes of cystitis (bladder inflammation) are infection and radiation.
Microscopic analysis of the urine during bladder infections will show
red blood cells along with white blood cells and possibly bacteria. The
patient typically will suffer from painful urination as well as urinary
frequency and urgency. Radiation cystitis can be seen in patients who
have received previous pelvic radiation. This is typically observed
after radiation treatment for prostate cancer. The bleeding can be quite
obvious and difficult to treat.
Prostate
Prostate Cancer
Due
to aggressive screening resulting in diagnosis at earlier stages,
nowadays hematuria is not commonly seen with prostate cancer. Before
modern screening, gross hematuria was quite common as prostate cancer
was often discovered at advanced stages.
BPH
While
the normal prostate has a high concentration of blood vessels, a
prostate with BPH has a significant increase in the density of blood
vessels.13 As a result, patients with BPH have a greater risk
of gross hematuria that can be frequent and, in some cases, severe
enough to cause clot formation and urinary retention.
Prostatitis
Hematuria
in the setting of prostate infection (prostatitis) will often occur
with a tender prostate on examination and worsening urinary symptoms.
Other Sources of Hematuria
Trauma
Injury
at any point along the urinary tract can cause hematuria. This can be
due to unplanned trauma, such as renal damage from a stab wound or
urethral injury from catheter insertion, or secondary to a procedure
such as laser surgery for stone disease.
Exercise-induced Hematuria
Hematuria
can be seen with strenuous exercise. It generally occurs with exercise
of longer duration and greater intensity. Once the activity is over, the
process resolves and has no long-term consequences.
Anticoagulation
Substantial
gross hematuria can be seen in patients taking medications that “thin
the blood” such as warfarin and heparin. However, the therapy itself
does not increase the risk for hematuria, unless levels of the
medication are well above therapeutic levels. Rather, anticoagulation
leading to hematuria uncovers urologic disease already present. One
study found urinary tract disease in 30% of patients on anticoagulation
therapy evaluated for hematuria.14 Importantly, the hematuria cleared in more than 90% of the patients after treatment.
EVALUATION OF PATIENTS WITH HEMATURIA
The
assessment of any patient with hematuria starts with a careful history
and physical examination. Identifying any family syndromes such as
sickle cell disease or cystic diseases of the kidney is an important
first step. It is also important to find out if the patient has any
other predisposing factors such as previous kidney stones or a history
of BPH. Hematuria in women during menstruation may be a contaminant, and
urinalysis should be repeated in between cycles.
Initial
laboratory tests consist of microscopic urinalysis and measurement of
serum creatinine (a blood test used to measure kidney function). The
urine should be analyzed for number and shape of red blood cells as well
as presence of white blood cells, bacteria, protein, and crystals. As
mentioned previously, abnormal red cells, casts, and significant
proteinuria indicate glomerular disease. White blood cells and bacteria
suggest infection, while crystals may be a result of stone disease. The
serum creatinine level is an indication of renal function, and an
elevated level in the face of glomerular disease requires prompt
referral to a nephrologist (physician who specializes in kidney
diseases).
GROSS HEMATURIA
Visible hematuria generally requires a full evaluation of the upper and lower urinary tracts.
Urine Cytology
Cytology
examines urine for cancerous cells of the urothelium (lining of the
urinary tract). The test has greater sensitivity for bladder cancer than
for cancers of the renal pelvis or ureter.
Radiologic Evaluation
Imaging
allows for the identification of renal tumors, stones, and significant
infections. Conventional radiologic evaluation was by intravenous
pyelogram (IVP). During this study, contrast dye is injected into a
vein, and a series of X-rays are taken as the dye is excreted by the
kidneys. Computerized tomography (CT) urography has largely replaced the
IVP. It provides a more detailed view of the upper urinary tract. For
patients with allergy to contrast dye or poor renal function, an
ultrasound of the kidneys, a magnetic resonance imaging (MRI), or a
retrograde pyelogram where dye is safely injected into the ureters and
kidneys can be performed.
Cystoscopy
Unfortunately,
radiologic imaging cannot identify small bladder tumors. Therefore, the
bladder is examined directly with a telescope attached to a camera
(cystoscopy). The smallest of tumors can be seen, as can stones or
prostatic bleeding. The entrance of each ureter into the bladder (the
ureteral orifices) is also examined, and in some upper tract disease,
blood can be seen spurting into the bladder (Figure 4).
Figure 4. Endoscopic View of Blood Entering the Bladder from the Right Ureteral Orifice
MICROSCOPIC HEMATURIA
Not
all patients with microscopic hematuria without symptoms need a
complete urologic assessment like that performed with gross hematuria.
However, patients with a higher risk for disease should undergo a full
urologic workup. These risks are as follows:2
- Smoking history
- History of gross hematuria
- History or urologic disease such as bladder cancer or stones
- History of bothersome urinary symptoms such as frequency and urgency
- Age older than 40 years
- Studies have shown no benefit to the screening of patients younger than 40 years15
- The risk of bladder cancer and other pathology increases with age16
- History of pelvic irradiation
- Occupational exposure to cancer-causing chemicals
- Abuse of pain medications (such as the anti-inflammatory aspirin, ketorolac, and ibuprofen)
- Previous urinary tract infections
If
none of the risk factors listed above are present, then radiologic
evaluation can be accompanied by urine cytology or cystoscopy. However,
if the cytology is suspicious, then a cystoscopy must be performed.
Patients
suspected of having benign transient microscopic hematuria should have
repeat urinalysis 48 hours after the offending activity is stopped.2
Examples include exercise-induced hematuria, menstruation, and trauma.
If the hematuria is still present, then a complete work-up is needed.
NEGATIVE WORK-UP
Some studies have shown that 10% or more of patients will have no abnormality found.1 However, disease can develop later and follow-up should be performed. This can consist of repeat urinalysis, cytology, and blood pressure measurement at 6, 12, 24 and 36 months.2 If any findings are suspicious then a complete work-up should be repeated. If the patient remains symptom free, then no further evaluation is needed.CONCLUSION
There are many causes of hematuria and although serious pathology may be associated more with gross rather than microscopic hematuria, any documented case should be properly evaluated. While the appearance of blood in the urine can be quite alarming, many of the causes are quite benign and treatable.ADDITIONAL RESOURCES
National Cancer Institute – www.cancer.gov
American Urological Association – www.urologyhealth.org
American Cancer Society – www.cancer.org
National Kidney Foundation – www.kidney.org
National Institutes of Health – www.nih.gov
National Institute of Diabetes and Digestive and Kidney Diseases – www.niddk.nih.gov
REFERENCES
1. “Hematuria.” UrologyHealth.org. Accessed 10 February 2008.
2. Grossfield
GD, Wolf JS, Litwin MS, Hricak H, Shuler CL, Agerter DC, Carroll PR.
Asymptomatic microscopic hematuria in adults: summary of the AUA best
practice policy recommendations. Am Fam Physician. 2001; 63: 1145-54.
3. Edwards
TJ, Dickinson AJ, Natale S, Gosling J, McGrath JS. A prospective
analysis of the diagnostic yield resulting from the attendance of 4020
patients at a protocol-driven haematuria clinic. BJU Int. 2006; 97: 301-5.
4. Alishahi
S, Byrne D, Goodman CM, Baxby K. Haematuria investigation based on a
standard protocol: emphasis on the diagnosis of urological malignancy. J R Coll Surg Edinb. 2002; 47: 422-7.
5. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA eds. Campbell’s Urology, 9th ed. Philadelphia: Saunders.
6. Fassett RG, Horgan BA, Mathew TH. Detection of glomerular bleeding by phase-contrast microscopy. Lancet. 1982; 26: 1432-4.
7. Schramek
P, Schuster FX, Georgopoulos M, Porpaczy P, Maier M. Value of urinary
erythrocyte morphology in assessment of symptomless microhaematuria. Lancet. 1989; 2: 1316-9.
8. Fassett RG, Horgan B, Gove D, Mathew TH. Scanning electron microscopy of glomerular and non glomerular red blood cells. Clin Nephrol. 1983; 20: 11-6.
9. Pollock
C, Liu PL, Gyory AZ, Grigg R, Gallery ED, Caterson R, Ibels L, Mahony
J, Waugh D. Dysmorphism of urinary red blood cells--value in diagnosis. Kidney Int. 1989; 36: 1045-9.
10. D’Amico. Clinical features and natural history in adults with IgA nephropathy. Am J Kidney Dis. 1988; 12: 353-7.
11. Coppo R, D’Amico G. Factors predicting progression of IgA nephropathies. J Nephrol. 2005; 18: 503-12.
12. Praga
M, Alegre R, Hernandez E, Morales E, Dominguez-Gil B, Carreno A, Andres
A. Familial microscopic hematuria caused by hypercalciuria and
hyperuricosuria. Am J Kidney Dis. 2000; 35: 141-5.
13. Foley SJ, Bailey DM. Microvessel density in prostatic hyperplasia. BJU Int. 2000: 85: 70-3.
14. Van Savage JG, Fried FA. Anticoagulant associated hematuria: a prospective study. J Urol. 1995: 153: 1594-6.
15. Froom P, Ribak J, Benbassat J. Significance of microhaematuria in young adults. Br Med J (Clin Res Ed). 1984; 288: 20-2.
16. Messing EM, Young TB, Hunt VB, Roecker EB, Vaillancourt AM, Hisgen WJ, Greenberg EB, Kuglitsch ME, Wegenke JD. Home screening for hematuria: results of a multiclinic study. J Urol. 1992; 148: 189-92.