Author: Dr John Maa University of California San Francisco 2008-07-29
Bariatric surgery: Overview on Weight Loss Surgery
Bariatric surgery is a term for operations to help promote weight loss.
Bariatric surgery: Overview on Weight Loss Surgery
Bariatric surgery is a term for operations to help promote weight loss.
Search terms: obese, bariatric surgery, weight loss, surgery, gastric bypass, stomach stapling, overweight, laparoscopic banding
Introduction:
Obesity is the condition in which fatty tissue stores are excessive. Obesity is associated with a number of co-morbid illnesses and an increased risk of premature death. The term overweight means that an individual has more body fat than is optimal. Morbid obesity is defined as being 100 lbs or more over ideal body weight or having a body mass index (BMI) of 40 or higher. BMI is a measure of body fat based on height and weight.
The
dramatic increase in obesity among Americans has become a critical
public health problem, especially among youths. Obesity is the second
leading cause of preventable death in the US. The
prevalence of obesity in America has been increasing from year-to-year
as is illustrated in the Department of Health and Human Services Center
for Disease Control and Prevention (CDC) U.S. Animated Obesity Map
(Figure 1). The number of overweight and obese Americans has increased almost continuously since 1960.
A number of environmental factors are associated with the development of obesity, including socioeconomic
status, race (more pronounced among Hispanic and Black populations),
and region of residence (highest in the Southeastern US). Recently,
the CDC report "Obesity Among Adults in the United States -- No Change
Since 2003-2004," found that obesity prevalence has plateaued, but
levels are still high –- at 34% of U.S. adults aged 20 and over.[i] An estimated 100 million adults in the United States are overweight or obese.
Central obesity
is also known as "apple-shaped" or "masculine" obesity, and occurs when
the primary deposits of fat are around the abdomen and upper body. Central obesity is associated with greater morbidity than peripheral obesity (fatty deposition on extremities and thighs), due to the increased metabolism of visceral fat. Central obesity is a leading risk factor for the development of the metabolic syndrome,
which is a combination of medical disorders that increases the risks of
developing cardiovascular disease and diabetes. This results from
elevated blood sugars and cholesterol, increased insulin secretion,
hypertension, and atherosclerosis.
What are the causes of morbid obesity?
The precise causes of morbid obesity are unknown, but are postulated to include the following:
Genetics:
Obesity can often be traced to genes, and abnormalities of neural or
hormonal transmitters to the hypothalamus or satiety center (the
neurologic center that controls the sensation of fullness) can cause
disruption of normal appetite tendencies.
Psychology: Psychologically induced oral dependency drives and emotional problems, and depression can lead to obesity.
Lifestyle:
Poor diet and low levels of daily activity are contributors to obesity.
Morbidly obese adults have been found to have a lower basal energy
expenditure.
What health conditions are related to being obese?
Obesity
is associated with many health consequences, such as high blood
pressure, respiratory and heart disease, lipid problems, and diabetes,
and has been implicated in some types of cancers. Obesity
can contribute to cardiac enlargement and impaired heart function,
irregular heart beat, and respiratory complications from the increased
weight of the chest wall. These factors can predispose patients to the development of coronary and cerebrovascular disease/stroke.
The list of co-morbid diseases include:
1) adult onset diabetes
2) sleep apnea
3) osteoarthritis
3) osteoarthritis
4) cancer
5) fatty liver disease
6) hypertension
7) high cholesterol and triglycerides (fat levels in the blood)
8) coronary artery disease
9) stroke
10) heart failure
11) venous thrombosis (blood clots) and venous stasis ulcers
12) pulmonary embolism (blood clots that travel to the lung)
13) heartburn
14) depression[ii]
Because of these associated medical problems, being obese can result in a shortened life span. One study suggested that the risk of death increased by 20- 40% among overweight persons, and by 200-300% among obese persons.[iii]
The term morbid obesity indicates the life-threatening seriousness of the condition. The death rate is greater for morbidly obese people than for people of average weight. Premature
death is much more common, and there is a 12-fold excess mortality in
morbidly obese men in the 25 to 34 year age group. Massively obese
patients—those who weigh more than twice the ideal weight – suffer
physical, emotional, social, and economic hardships.
What is body mass index?
The body mass index (BMI) is a standard way to define overweight, obesity, and morbid obesity, and is a measure of body fat based on height and weight that applies to both adult men and women. The average BMI in American society is 25. A BMI of 25 or more is considered overweight, and 30 or more to be obese. Morbid obesity is defined as either a) body weight 100 lbs over ideal, or 2) a BMI over 40. Surgical
intervention is currently indicated for patients with a BMI over 40, or
a BMI over 35 with recognized comorbid conditions.
The BMI is calculated as:
In International units:
BMI = Weight in KILOGRAMS /(Height in METERS)2
In English units:
BMI = Weight in POUNDS x 703 /(Height in INCHES)2
A BMI calculator can be found at http://www.nhlbisupport.com/bmi/
The current consensus definitions establish the following values:[iv]
- A BMI less than 18.5 is considered underweight
- A BMI of 18.5–24.9 is considered normal weight
- A BMI of 25.0–29.9 is considered overweight
- A BMI of 30.0–39.9 is considered obese
- A BMI of 40.0 or higher is considered severely (or morbidly) obese
- A BMI of 35.0 or higher in the presence of at least one other significant comorbidity (diabetes mellitus, coronary artery disease, hypertension, sleep apnea, or degenerative joint disease) is also classified as morbid obesity.[v]
The 5th and 6th BMI categories above are also the criteria for weight loss surgery.
Consideration
of a patient's body shape, height, and muscularity should also be taken
into account, since muscle is more dense than fat. If one is muscular, then other means of determining body fat should be employed. A
report in the Journal of the American Medical Association demonstrated
that 97% of players in the National Football League are technically
overweight and more than 50% are obese.[vi]
Why Bariatric Surgery (Weight Loss Surgery)?
For people who are overweight or obese, but not morbidly obese, diet and exercise are the safest and best way to reduce weight and reduce health risks. If you are just overweight, the risk of bariatric surgery outweighs the risk of premature death and future medical problems.
However, for
men who are less than 100 pounds overweight and women who are less than
80 pounds overweight, weight loss surgery has been shown to be the most
effective treatment.[vii] If
you are morbidly obese, or obese with at least one co-morbidity, over
your lifetime you are at higher risk of dying prematurely or suffering
from worsening health problems, and the risk of bariatric surgery is
justified
Thus
a gastric bypass is offered to reduce your caloric intake and have been
unable to achieve the desired weight through diet and exercise. Gastric
bypass surgery can improve the quality of life not only because of an
improvement in appearance and an increase in mobility, but because it
can also reduce the severity of health problems from which overweight
people are prone to suffer.
What are the indications for bariatric surgery?
Obesity surgery was throughly evaluated by a consensus panel assembled by the US National Institutes of Health (NIH) in 1990. The
consensus statement issued by this multidisciplinary panel of surgeons,
internists, and public health specialists is the major defining
standard for the care for obesity surgery.
The NIH created the following guidelines for bariatric surgery:
- A BMI of 40.0 or higher is considered severely (or morbidly) obese
- A BMI of 35.0 or higher in the presence of at least one other significant co-morbidity is also classified as morbid obesity.[viii]
The
panel also reviewed the existing data at that time and concluded that
only the vertical banded gastroplasty and Roux-en-y gastric bypass could
be recommended. These surgical approaches are discussed below.
Are there any alternatives to bariatric surgery?
The
standard approach to therapy for obesity begins with reducing diets and
medical counseling, but unfortunately these measures are often
unsuccessful in patients with severe obesity. The weight that is rapidly
lost is often quickly regained.
Non-surgical options for the treatment of morbid obesity include
1) diet modification
2) exercise programs
3) medications and
4) social support programs
To
date, non-surgical treatments have not been very effective in treating
obesity, regardless of the approach used, with high rates of recurrence,
up to 90%.[ix] No
dietary approach has achieved uniform long-term success for the
morbidly obese—many can lose weight temporarily but it then regain. There are currently no effective pharmacologic agents to treat obesity. Surgery
is currently accepted as the treatment approach producing the greatest
and longest-lasting success in achieving weight loss.
How safe is bariatric surgery?
Bariatric surgery is often portrayed as a high risk procedure. While
the surgery is, indeed, more risky than many other operations, much of
the risk relates to the patient’s obesity rather than to the actual
operation itself. Nonetheless, surgery has inherent risks including significant early and late morbidity and perioperative mortality. An
extensive review of 361 bariatric surgery studies including over 85,000
patients found that the total mortality within the first 30 days of
surgery was 0.28%, and the total mortality during the period from 30
days to 2 years was 0.35%.[x]
Surgery for obesity is more effective than medical management, producing greater weight loss. A trial 80 adults with mild to moderate obesity (BMI 30-35 kg/m2)
randomized patients to either adjustable gastric banding or an
intensive medical (non-surgical) program and found that at 2 years, the
surgical group had lost 87.2% of excess weight, while the non-surgical group lost only 21.6%.[xi] as well as improvements in quality of life and co-morbidities have also be found. 12 The continued weight loss after gastric bypass has been documented to extend for as long as 10 years after initial operation. [xii] Surgery was found to be more effective than non-surgical weight loss in terms of reducing both weight and health risks.[xiii]
Is bariatric surgery appropriate for children and teenagers?
The
number of U.S. children having obesity surgery has increased rapidly in
recent years, at a pace that could result in more than 1,000 such
operations in 2008. The procedure remains far more common
in adults, but preliminary data suggests it may be slightly less risky
in teens, according to an analysis of data on 12- to 19-year-olds who
had obesity surgery from 1996 through 2003. Adolescents
should be strongly encouraged to attempt dietary and exercise
interventions first, and bariatric surgery should only be undertaken
after careful consideration by the patient, family, physician, and
medical center.
What steps must be undertaken before I can have bariatric surgery?
Before
bariatric surgery is offered, a potential patient must undergo an
extensive evaluation by a multidisciplinary team of providers to address
all aspects of the complex medical, surgical, psychological, and nutritional issues.
Potential
patients must commit to compliance with the diets postoperatively, and
comply with lifelong follow-up for potential ongoing medical conditions. Marked
anemia can develop after bariatric surgery if vitamin supplementation
is inadequate, and often results from the failure of coupling of vitamin
B12 to intrinsic factor or insufficient stores of folate.
What additional procedures might be necessary in conjunction with bariatric surgery?
Additional surgical procedures are sometimes recommended at the same time, or after, bariatric surgery. Approximately
30- 40% of patients who undergo gastric bypass will subsequently form
gallstones, thus many surgeons recommend removal of the gallbladder at
the time of bariatric surgery.
If
excess fat or skin is localized in an area, a simultaneous or staged
panniculectomy (liposuction) may be performed- especially for those
patients who develop a hernia in their incision after marked weight
loss.
How long does it take to lose weight?
Most
patients observe the majority of their weight loss within one year and
achieve a stable weight by the end of the second year. Their
weight loss plateaus once their caloric intake and caloric expenditure
are balanced. On average, there is a reported loss of one half to two
thirds of excess weight within 1 to 1.5 years. This
weight loss completely corrects insulin dependent diabetes in most
cases, and most patients no longer require insulin after bariatric
surgery. Many patients have resolution of their headaches
from a reduction of cerebrospinal fluid pressure elevation, and many
cases of obstructive sleep apnea and gastroesophageal reflux also
resolve.
History of Bariatric Surgical Therapy:
The
first operations to control obesity were small bowel bypasses, which
rely on malabsorption alone – that is, surgically changing the stomach’s
anatomy to selectively prevent it from absorbing nutrients. The first
operation for obesity that gained widespread acceptance—the jejunoileal bypass --
is no longer performed as it was associated with an unacceptably high
rate of liver failure (in up to 10% of patients), renal failure, and
metabolic complications. Many surgeons believe that all jejunoileal bypass procedures should be reversed to prevent cirrhosis, and conversion to one of the bypass procedures described below if weight loss is to be maintained.
Current Surgical Therapy:
The
modern era of gastric procedures for weight loss was based on the
observation that some patients who underwent stomach ulcer surgery lost
weight afterwards. In 1969, investigators reported the
results of weight loss following reduction of the stomach to the size of
a small pouch. This technique was simplified with the use of stapling
instruments.
Current surgical procedures for weight loss have three essential approaches:
(1) the restriction of food intake (restrictive procedures)
(2) anatomic modification of the gastrointestinal tract to create selective malabsorption (poor absorption) of nutrients (malabsorptive procedures)
(3) a combination of both restrictive and malabsorptive procedures
The two most popular current surgical procedures for weight loss include gastric bypass and adjustable gastric banding. Other operations that have been done include vertical banded gastroplasty and biliopancreatic diversion and duodenal switch
but are falling out of favor due to loss of effectiveness (vertical
banded gastroplasty) and a high incidence of complications
(biliopancreatic diversion and duodenal switch).
Gastric Bypass
A gastric bypass is an effective procedure that achieves weight loss by both restrictive and malabsorptive mechanisms. The Roux-en-Y gastric bypass has become popular over the past decade as it results in substantial weight loss, but the long-term physiologic consequences are still being evaluated closely through multicenter research studies. It is an irreversible procedure. In this procedure, a portion of the small intestine (Roux-en-Y loop) is joined with a small portion of the upper stomach to create a small pouch (approximately 15 mL volume). The remainder of the stomach, duodenum, and proximal jejunum are excluded from food contact. In the standard procedure, the digestive secretions from the bile duct system and pancreas enter the jejunum 40- 50 cm from the stomach, resulting in malabsorption.
To promote greater weight loss, the procedure can be modified as a long limb gastric bypass (100 to 150 cm from the stomach) and is often considered in the superobese (BMI > 50). The procedure is well tolerated by most patients and is effective in achieving weight loss.[ix] Laparoscopic gastric bypass requires a high level of technical skill not possessed by most general surgeons.
The Roux-en-Y bypass is more common and considered less complicated
than the biliopancreatic diversion bypass, since Roux-en-Y does not remove portions of the stomach.
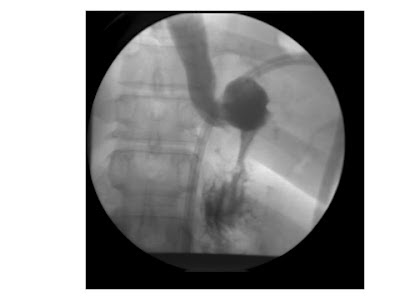
The
most feared complication after a gastric bypass is a postoperative
gastric leak with peritonitis resulting from bacterial escape into the
abdomen. It can be difficult to recognize due to the marked amount of
abdominal wall fatty tissue. Any signs of tachycardia,
fever, tachypnea, and leukocytosis should be carefully explored in a
postoperative gastric bypass patient. If suspicious, immediate reoperation should be performed.
Specific complications associated with gastric bypass include:
1) staple failure or disruption
2) anastomotic leaks and peritonitis
3) acute gastric dilatation
4) marginal ulceration
5) dumping syndrome (food moves too rapidly through the intestinal tract resulting in diarrhea)
6) stomal stenosis (narrowing of the connection between the stomach and intestines) which may require endoscopic dilation
Common postoperative complications such as wound infection, pulmonary embolism, hernia, and bowel obstruction are also observed.
Gastric Banding
Gastric
banding (also known as LAP BAND) is a popular alternative to gastric
bypass that is also reversible. It is commonly performed
laparoscopically and is less technically demanding than a laparoscopic
gastric bypass. Food intake is limited by the placement
of a constricting ring around the upper portion of the stomach, dividing
the stomach into a small portion above the band (a 5-15 mL pouch) and a
much larger portion below the band. The band can be
adjusted by inflation of a reservoir to allow gradual regulation of the
diameter of the stoma (the pouch outlet to the intestine). Laparoscopic
gastric banding has been shown to result in acceptable weight loss and
reductions in co-morbidities, but in some patients both the degree of
weight loss and reduction in co-morbid conditions are less than that
with gastric bypass.
Multi-center long-term results in the US are still being investigated.[xiv]
Since this is a restrictive procedure, gastric banding avoids the
problems associated with malabsorptive techniques such as malnutrition
and dumping syndrome. Specific LAP BAND complications include splenic or
esophageal injury, esophageal dilation, wound infection, band slippage
or erosion, reservoir deflation, persistent vomiting, and acid reflux.[xv]
Vertical Banded Gastroplasty
The vertical banded gastroplasty (VBG) is a restrictive procedure that limits the amount of food a patient is able to ingest. VBG is infrequently performed today due to the failure of many patients to achieve sustained weight loss,[xvi] and undesirable side effects such as heartburn and vomiting (reported in up to 38% of patients). In
this procedure, the stomach is divided by a stapler along the lesser
curvature to create a small pouch. A band or ring of silicone or
polypropylene mesh is placed through a hole in the stomach to limit the
size of the pouch outlet (stoma). Reasons for the failure
of this procedure may include dilation and enlargement of the gastric
pouch, stomal stenosis, staple line failure, and problems related to the
non-adjustable band.[xiv]
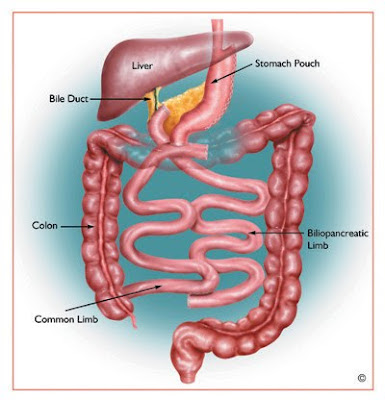
Biliopancreatic Diversion With and Without Duodenal Switch
The biliopancreatic diversion is a less common and more complex procedure than the Roux-en-Y gastric bypass. It is less widely used, as there is a perceived greater risk of nutritional deficiencies. It can be performed both with and without the "duodenal switch." It
includes a malabsorptive procedure that involves removal of a portion
of the stomach and a long “Roux-en-Y” (where the small intestine is
re-fashioned into a “Y” shape). The small intestine is divided, and the
distal end (alimentary, or Roux-en-Y, limb) is connected to the gastric
remnant. The proximal (biliopancreatic) limb of intestine is connected
to the alimentary limb 50-100 cm from the ileocecal valve.
As
an alternative, the procedure may also be performed with a "duodenal
switch," in which the Roux limb is anastomosed to the duodenum rather
than the stomach, and a linear (sleeve) gastrectomy, in which a
significantly greater portion of the stomach is removed leaving a narrow
tube based on the lesser curvature of the stomach.
Weight
loss following biliopancreatic diversion is achieved by both
restriction and selective malabsorption of nutrients. Biliopancreatic
diversion may be the most effective in producing weight loss but is
technically difficult to perform, particularly laparoscopically, of
significantly higher risk, and may produce marked malnutrition and
vitamin deficiencies.[xvii] The advantage is that there is no blind intestinal limb.
Diagram:
Intra-Gastric Balloon
The
intent of the intra-gastric balloon is to create a sense of earlier
satiety by filling a portion of the stomach from within (a restrictive
procedure). It was developed to offer a nonsurgical and reversible approach to obesity control. However,
the intra-gastric balloon has been removed from the US market after
several publicized deaths resulted from obstruction secondary to the
passage of a partially digested intra-gastric balloon.
In
Europe and elsewhere in the world, the intra-gastric balloon is still
used temporarily, for periods of up to 6 months, as a “bridge” to bring a
severely obese patient down to a weight where they can undergo a
permanent bariatric operation with less risk. It must be removed within 6 months, otherwise digestion and resulting complications may occur. It
is therefore utilized primarily for mild cosmetic weight loss, and also
to help patients lose weight prior to one of the previously described
weight loss surgeries.
What if the initial procedure is unsuccessful?
A subset of patients will not achieve the desired weight loss postoperatively. Most patients who fail surgery do so from excessive calorie consumption relative to calories burned through activity. Attention
is first directed at determining whether the patients have continued to
ingest large amounts of sugar-containing beverages, or by preferential
ingestion of foods with a high caloric density.
After this has been excluded, patients can be considered as candidates for revisional surgery. However,
reoperation can be very difficult due to adhesions, scarring, and the
altered anatomy, and the attendant perioperative risks are much higher
than with the first procedure. Often the best results are
achieved by conversion to a Roux-en-Y gastric bypass, though the use of a
modified partial biliopancreatic diversion can also be considered.
Newer Surgical Therapy and Endoscopic Therapy:
Vertical Sleeve Gastrectomy
Vertical gastrectomy (VG) is the
restrictive component of a more extensive mixed restrictive and
malabsorptive operation, the biliopancreatic diversion with duodenal
switch.[xviii] VG
was first performed as a distinct operation in 2001 with the intent to
remove approximately 90% of the stomach leaving a narrow tube or
“sleeve” which greatly reduces the stomach volume creating satiety, or
the sensation of fullness. The procedure minimizes the
complications of dumping and ulcer formation, but sometimes requires
completion of the second stage of the procedure to promote
malabsorption.
There
are currently 15 published reports in the surgical literature
describing short-term outcomes in 775 patients after sleeve gastrectomy.[xix] This
procedure has been shown to result in significant weight loss, with
excess weight loss ranging from 33% to 83%. Rates of resolution of
co-morbid conditions such as diabetes, hypertension, hyperlipidemia, and
sleep apnea within 12- 24 months are comparable to results of other
restrictive procedures.[xx] Similar
to other forms of gastroplasty, the perioperative risk for sleeve
gastrectomy appears to be relatively low, even in high-risk patients.
Published complication rates range from zero to 24% with an overall
reported mortality rate of 0.39%.[xviii]
Neuromodulation
The vagus nerve is involved in the control of digestion, intestinal motility, and feelings of fullness. Under
investigation is a surgically implanted unit that modulates the
electrical impulses of this nerve with the intent of slowing the rate of
stomach emptying to promote a sense of satiety. The initial weight loss has been inferior to established bariatric operations. Weight loss of 20 lbs at 20 weeks, and 36.1 lbs at 1 year, have been reported, but long-term data is pending.[xxi] The cost and replacement of the battery unit for this device has been recognized as a significant limitation.
Investigational Endoluminal or Endoscopic Therapies on the Horizon
Less
invasive approaches to surgery are being investigated, which utilize
endoscopes introduced through the mouth to achieve weight loss. Active areas of research involve approaches that include:
1) stapling from within the stomach to restrict the volume of the stomach
2)
lining the intestinal tract with a sheath to prevent contact between
food and digestive enzymes and thereby reduce absorption of food
3) ribbons, gels, or polymers which can fill the stomach to restrict volume
4) endoscopically implanted neuromodulation devices.
Diagrams:
EndoBarrier™ - http://www.gidynamics.com/endobarrier_technology
Summary:
For people who are overweight, diet and exercise are the safest way to achieve weight loss. For those who are morbidly obese or with significant co-morbidities, bariatric surgery is the most effective means to achieve weight loss to optimize health. Individuals considering bariatric surgery should discuss the risks and
possible benefits carefully with their physician, as surgery does
present associated risks and long-term consequences. Most bariatric surgeons
think that the operations represent only one part of the approach to
treating obesity and are most successful in conjunction with lifelong
behavioral and dietary changes.
Useful Web sites:
United States Animated Obesity Map showing state-by-state trends from 1985-2006.
American Society for Bariatric Surgery
http://www.asbs.org
http://www.asbs.org
American Society of Bariatric Physicians
Journal of the American Medical Association: Bariatric Surgery
American Society for Metabolic & Bariatric Surgery: The Story of Surgery for Obesity: A Brief History and Summary of Bariatric Surgery
Cleveland Clinic Health Information Center: Surgical Options for Severe Obesity
Medline Plus: Weight Loss Surgery
NIH (National Institute of Diabetes and Digestive and Kidney Diseases): Gastrointestinal Surgery for Severe Obesity
Society of American Gastrointestinal and Endoscopic Surgeons: Morbid Obesity
American Society for Metabolic & Bariatric Surgery: Benefits of Bariatric Surgery
Related articles:
Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA 2005; 294: 1909-1917.
Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA 2005; 294: 1918-1924.
Zingmond DS, McGory ML, Ko CY. Hospitalization before and after gastric bypass surgery. JAMA 2005; 294: 1918-1924.
References:
[i] Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States – no statistically significant change since 2003-2004. NCHS Data Brief 1, November 2007. 8pp. http://www.cdc.gov/nchs/data/databriefs/db01.pdf
[ii] Bray GA (2004). "Medical consequences of obesity". J. Clin. Endocrinol. Metab. 89 (6): 2583-9.
[iii] Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Holleenbeck A, Leitszmann MF. Overweight, Obesity, and Mortality in a Large Prospective Cohort of Persons 50 to 71 Years Old. NEJM 2006; 355: 763-778.
[iv] World
Health Organization Technical report series 894: "Obesity: preventing
and managing the global epidemic.". Geneva: World Health Organization,
2000.
[v] NIH National Institute of Diabetes and Digestive and Kidney Diseases). Gastrointestinal surgery for severe obesity. Accessed 7th February 2008. http://win.niddk.nih.gov/publications/gastric.htm
[vi] Harp JB, Hecht L. Obesity in the National Football League. JAMA; 293: 1061-62.
[vii] Waseem T, Mogensen KM, Lautz DB, Robinson MK. Pathophysiology of obesity: why surgery remains the most effective treatment. Obes Surg 2007; 17(10): 1389=98.
[viii] NIH National Institute of Diabetes and Digestive and Kidney Diseases). Gastrointestinal surgery for server obesity. Accessed 7th February 2008. http://win.niddk.nih.gov/publications/gastric.htm
[ix] The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH Publication No. 00-4084 2000.
[x] Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 2007; 142(4): 621-32.
[xi] O’Brien PE, Dixon JB, Laurie C, Skinner S, Proletto J, McNeill J, Strauss B, Marks S, Schachter L, Chapman L, Anderson M. Treatment
of mild to moderate obesity with laparoscopic adjustable gastric
banding or an intensive medical program: a randomized trial. Ann Intern Med 2006; 144: 625-33.
[xii]
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pries W, Fahrbach K,
Schoelles K. Bariatric surgery: a systematic review and meta-analysis.
JAMA 2004; 292: 1724-1737.
[xiii] Colquitt J, Clegg A, Loveman E, Royle P, Sidhu MK. Surgery for morbid obesity. Cochrane Database Syst Rev 2005; 4: CD003641.
[xiv] Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA 2004; 292: 1724-1737.
[xv] Fried M, Miller K, Kormanova K. Literature review of comparative studies of complications with Swedish band and Lap-Band. Obes Surg 2004; 14(2): 256-60.
[xvi] Crookes PF. Surgical treatment of morbid obesity. Annu Rev Med 2006; 57:243-64.
[xvii] Scopinaro
N, Gianetta E, Adami GF, Friedman D, Traverso E, Marinari GM, Cuneo S,
Vitale B, Ballari F, Colombini M, Baschieri G, Bachi V. Biliopancreatic diversion for obesity at eighteen years. Surgery 1996; 119(3): 261-8.
[xviii] Lee
CM, Cirangle PT, Jossart GH. Vertical gastrectomy for morbid obesity in
216 patients: report of two-year results. Surg Endosc 2007.
[xix] American Society for Metabolic & Bariatric Surgery: Position Statement on Sleeve Gastrectomy as a Bariatric Procedure. http://www.asbs.org/Newsite07/resources/sleeve_statement.pdf. Accessed 6 February 2008.
[xx] Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic
sleeve gastrectomy as an initial weight-loss procedure for high-risk
patients with morbid obesity. Surg Endosc 2006; 20(6):859-63.
[xxi] Bohdjalian A et al. One-year experience with Tantalus. Obes Surg 2006; 16(5): 627-34.