Author: Anne Peters, MD, FACP, CDE Director, USC Clinical Diabetes Programs Los Angeles, CA
2010-10-11What is type 1 diabetes?
2010-10-11What is type 1 diabetes?
Type 1 diabetes is a disease that often starts in childhood and was
previously known as “juvenile onset” diabetes, but we now know that it
can start at any age. People with type 1 diabetes have stopped making
insulin from the beta-cells in their pancreas, so they depend on insulin
injections for life. Type 1 is much less common than type 2 diabetes
(1-2 million individuals have type 1 diabetes in the United States
compared to 19 million who have type 2), but it often has a much more
sudden start, with patients (particularly children) becoming very ill
and requiring hospitalization for treatment. Although not curable, type
1 diabetes is very treatable with the appropriate care.
In some ways, type 1 diabetes is a simple disease. It is an autoimmune process which means it is a process in which the body’s infection-fighting response incorrectly destroys its own cells; in this case the infection-fighting response destroys the insulin-producing cells in the pancreas (the beta-cells). Therefore patients with type 1 diabetes stop making their own insulin and are completely dependent on insulin for life. (Although as with all diseases there are shades of gray; often early in type 1 diabetes people can make a little bit of their own insulin, with this gradually going away over time). Type 1 diabetes is different from patients with type 2 diabetes, who have both insulin resistance and insulin deficiency and have more treatment options than insulin alone.
An unusual increase in thirst is often a sign of developing type 1 diabetes.
The classic example of someone who gets type 1 diabetes is a skinny kid
who over the course of a month becomes very ill, with weight loss and
an increasing, insatiable thirst. Usually there is no family history of
diabetes, so the parents don’t know to watch out for it. By the time
the child is brought to the doctor or the emergency room they are very
sick, usually with a condition known as diabetic ketoacidosis or DKA.
DKA happens when there is so little insulin in the body that the body
breaks down fat for fuel. Too much fat breakdown leads to the excessive
build up of ketones (a by-product of your body burning stored fat) in
the blood and this can cause serious problems if not treated.
The diagnosis of diabetes is often a complete and devastating shock.
Suddenly everything must be learned about taking care of diabetes. All
of the information about what to eat, and what high and low blood sugar
levels mean, and how to test blood sugars and give insulin injections
must be assimilated over the course of a week. Usually this week is
spent in the hospital, teaching the child and their family about the
basics of diabetes and how to deal with it once they are sent home.
This is a lot to deal with all at once, and the child and everyone in
their family needs lots of help and support as they learn to cope with
the diagnosis.
There is also another, more slowly
starting form of type 1 diabetes that happens in adults. This is called
latent autoimmune diabetes of the adult (LADA). It is often confused
with type 2 diabetes, because both can happen in older patients (my
oldest patient with newly diagnosed LADA or type 1 diabetes is 93 years
of age). It is a more gradual process than is seen in childhood onset
type 1 diabetes and initially is often treated like type 2 diabetes,
with a slow evolution to insulin dependence.
What is the role of the pancreas?
As described above, type 1 diabetes means that the insulin secreting
cells in the pancreas, the beta-cells, are destroyed. This usually does
not mean that the whole pancreas stops working (unless you have had it
surgically removed), just the little cells that make insulin.
The pancreas itself is a squishy organ that is located in the middle of
the abdomen. Most of what the pancreas does is to secrete enzymes into
the intestines when food is eaten. These enzymes help digest food. If
the pancreas is removed or destroyed by a disease like cystic fibrosis,
it is necessary to take enzyme pills every time food is eaten to help
with digestion.
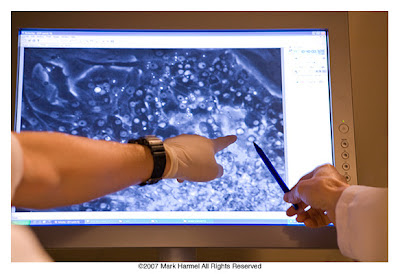 |
| Confocal microscope images of pancreatic islet cells at the Larry L. Hillblom Islet Research Center located at UCLA. |
Little
islands of cells are scattered in the tissue that makes the digestive
enzymes in the pancreas. These cell clusters are called islet cells.
They make substances called hormones that are released into the blood
stream. The main cells in the islets are beta-cells which make insulin
and amylin, plus alpha cells which make glucagon (a hormone that
increases blood sugar levels, instead of lowering it like insulin).
There are also delta-cells, which make other hormones that we don’t know
much about.
In type 1 diabetes the body makes a protein –
called an antibody – that is normally made to destroy unwanted bacteria
in our bodies. In this case the body is fooled into making antibodies
against a part of itself, the beta-cells. When these antibodies attach
to the beta-cells they cause the cells to die. Interestingly these
antibodies are so specific that they only attack the beta cell, which is
why early in the disease process glucagon is still released from the
alpha cells. For some reason the alpha cells lose their ability to
release glucagon after about five years, which makes people more
susceptible to low blood sugar reactions.
People don’t lose all
of the function of their beta-cells all at once, even if it sometimes
seems that way. What happens is that the cells are slowly killed off
over time. At the point where about half of the beta-cells are lost
blood sugar levels start to increase. Sometimes, when someone gets a
virus or another illness, they become resistant to the action of
insulin. This happens in everyone, but if the beta-cells are partly
destroyed your blood sugar levels can climb and you can quickly become
quite ill.
Sometimes people have surgery to remove most or all
of their pancreas. This not only gets rid of the beta-cells, but also
the alpha cells. People wake up from removal of their pancreas with
sudden, very brittle diabetes. These people functionally have a form of
type 1 diabetes, although some people categorize it differently because
it isn’t due to an autoimmune process.
What is the role of measuring antibodies in the blood?
The antibodies that circulate in the blood and destroy the beta-cells
can be measured. Measurement of antibodies can be helpful to determine
the type of diabetes and confirm the diagnosis. In children with new
onset type 1 diabetes three antibodies are measured, and are often
positive at the time of diagnosis: anti-islet cell antibodies,
anti-insulin antibodies and anti-GAD antibodies. In adults with new
onset type 1 diabetes, anti-GAD antibodies are often positive (and they
remain positive over time). Measurement of anti-GAD antibodies can be
helpful in distinguishing type 1 from type 2 diabetes, especially when
an adult without typical risk factors develops diabetes (see below).
What is latent autoimmune diabetes of the adult (LADA)?
Older individuals who develop diabetes, particularly those who are not
overweight and who do not have a family history of type 2 diabetes
should be tested to see if they really have slowly evolving type 1
diabetes. The blood test for this is called an anti-GAD antibody. If
the level is elevated it might mean that the beta-cells are being slowly
destroyed and treatment with insulin may be required. Some call LADA
type 1.5 diabetes, since it can start as a confusing intermediate
between type 1 and type 2 diabetes. However, since it is a slowly
destructive process of the beta-cells, LADA is the more specific term.
Zippora Karz, New York City Ballet soloist who was diagnosed with Type 1 diabetes at 21.
Which adults should be tested for type 1 diabetes (LADA)?
Adults (from age 18 up) who develop diabetes and who are lean to normal
weight, not from a high risk ethnic groups for type 2 diabetes (Latino,
African American, Asian American, American Indian, Pacific Islander),
and without a family history of type 2 diabetes are more likely to have
type 1 diabetes. Also, not responding well to oral medication used for
the treatment of type 2 diabetes may mean the diagnosis of type 1
diabetes (LADA) is more likely.
What happens after the diagnosis of diabetes?
First find a healthcare team. The American Diabetes Association lists certified diabetes education programs
that can provide education and resources. Additionally, if possible
find an endocrinologist. Type 1 diabetes is fairly uncommon and most
doctors in general practice only have a few individuals with the
disease. Treating someone with type 1 diabetes means interpreting data,
reviewing blood sugar levels, providing insulin doses, and counting
carbohydrates. It means using the newest technology available for
monitoring and treating the disease. Often the physician isn’t the best
person for doing a lot of the day-to-day management — working with a
diabetes educator is often the best method – but normally general
practice doctors don’t have a diabetes educator and a dietitian working
with them. An endocrinologist usually will have both.
lists certified diabetes education programs
that can provide education and resources. Additionally, if possible
find an endocrinologist. Type 1 diabetes is fairly uncommon and most
doctors in general practice only have a few individuals with the
disease. Treating someone with type 1 diabetes means interpreting data,
reviewing blood sugar levels, providing insulin doses, and counting
carbohydrates. It means using the newest technology available for
monitoring and treating the disease. Often the physician isn’t the best
person for doing a lot of the day-to-day management — working with a
diabetes educator is often the best method – but normally general
practice doctors don’t have a diabetes educator and a dietitian working
with them. An endocrinologist usually will have both.
How is insulin used in type 1 diabetes?
Type 1 diabetes is treated with insulin injections designed to mimic
the action that the beta-cells in the pancreas once performed. Someday
there may be other ways to treat and even cure type 1 diabetes, but for
now the only way to get insulin into the body is with injections (or
through an insulin pump). No other way works well enough. Oral insulin
doesn’t work because insulin in the stomach is destroyed by acid. The
recent option of inhaled insulin has been taken off the market.
Fortunately current technology has made the needles on insulin syringes
and pens very small so that injections hardly hurt, which makes giving
shots easier than it used to be.
General Philosophy About Insulin
In someone who doesn’t have diabetes, the pancreas is able to make just
the right amount of insulin to mesh with the food that is eaten and the
body’s own production of sugar. The pancreas makes a little bit of
insulin all of the time, 24 hours a day. This is called the basal
insulin level. The basal insulin is the amount of insulin needed to
compensate for the sugar made by the liver. In theory, if no food is
eaten the basal insulin level keeps the blood sugar levels
constant—neither too high or to low. When someone without diabetes
doesn’t eat, the blood sugar level stays stable because of the interplay
of normal hormones and the production of sugar from the liver.
Every time a person eats carbohydrate (meaning sugar, since all
starches and simple sugars are sugar in the blood) the blood sugar level
goes up. This tells the pancreas to release more insulin. The more
carbohydrate (sugar) that is eaten, the more insulin the body makes.
This is called the meal-time insulin or bolus insulin. Thus, in someone
without diabetes, the body has a low, basal level of insulin and
releases premeal bursts or boluses of insulin. This keeps the blood
sugar level normal all day long.
This graph demonstrates how a healthy pancreas releases a balanced amount of insulin to cover the basal and bolus requirements.
In someone with type 1 diabetes, the pancreas makes no insulin, and insulin shots are given to mimic what the normal pancreas would do. The goal is to match the pattern of giving a basal insulin and then doses of insulin each time food is eaten. The nondiabetic pancreas knows what the blood sugar level is every second. To mimic this, the diabetic patient must test the blood sugar level before every meal and at bedtime (and often before snacks and exercise).
The goal in treating type 1 diabetes is to adjust the insulin to a
person’s lifestyle, rather than the other way around. Some diabetes
patients have fixed doses of insulin or use fixed mixtures of fast and
slow insulin such as 70/30 or 75/25, but these insulins provide very
little flexibility. With the proper care diabetes doesn’t need to be a
lifestyle limiting disease; people with type 1 diabetes have won Olympic
gold medals and are professional race car drivers.
 |
| Indy Lights driver Charlie Kimball manages the twists and turns of the race course as well as his blood sugar. |
What are the types of insulin?
To understand the use of insulin it is important to understand the
types of insulin that are available. In the old days, most insulin came
from animal sources like pork or beef. Now, nearly all insulin is
scientifically formulated to be identical to human insulin.
The most basic form of human insulin is regular insulin. This insulin
is clear in color and is just like the insulin that comes from the
pancreas. The problem with regular insulin is that it forms clumps
under the skin after injection, and these clumps slow down how quickly
it gets absorbed. To get around this absorption problem, drug companies
changed the structure of the insulin a little bit, so it is absorbed
more reliably and more quickly or slowly. These changed insulin
molecules are called insulin analogues and have revolutionized our
ability to treat people with type 1 diabetes because they can more
closely approximate normal insulin secretion.
Lispo Humalog, aspart Novolog and glulisine Apidra
are the three rapid acting insulin analogues. After injection, they
start to work quickly, which is the way a normal pancreas would
function. Glargine Lantus and detemir Levemir
are long acting insulin analogues, which stay in the body as a steady,
basal insulin. People with type 1 diabetes typically use a combination
of both, which helps them have less weight gain, fewer low blood sugar
reactions, and somewhat better glucose control than those on the older
insulins. People get their proper insulin doses either through multiple
injections throughout the day or from an insulin pump.
Insulin
is categorized by how fast it works it the body, how soon it peaks and
then how long it lasts. Notice how rapid acting insulins have a rapid
rise and fall while longer acting insulin builds more slowly to a stable
baseline before declining.
What is the “Honeymoon” Phase?
Insulin requirements may end up being less during the first few months
of having diabetes, something known as the “honeymoon phase,” in which
the beta-cells seem to recover a little bit of the ability to make
insulin and decrease how much insulin must be given by injection.
Keeping diabetes under good control from the start can prolong the
body’s ability to make its own insulin for several years, and although
insulin shots are still required, it is often easier control the blood
sugars when the body can participate.
How Is An Intensive Insulin Regimen Created?
To create a regimen that is similar to the body’s natural patterns,
patients must test their blood sugar levels before each meal and give
rapid acting insulin in order to deal with the carbohydrate eaten at
that meal. In addition, the insulin dose must be adjusted if before
eating the blood sugar is too high or too low. The once or twice a day
dose of long acting insulin creates a base to help keep the blood sugar
level steady overnight, which leads to a more normal blood sugar.
The
long acting insulin is given once (usually glargine [Lantus]) or twice
(usually detemir [Levemir]) daily to provide a base, or basal insulin
level. Rapid acting (RA) insulin is given before meals and snacks. A
similar profile can be provided using an insulin pump (discussed later
in this Knol) where rapid acting insulin is given as the basal and
premeal bolus insulin.
What are the blood sugar targets?
Blood
sugar is the measurement of glucose levels in the blood. Depending on
where in the world you live, the units for blood sugar levels are
different. In the United States it is reported as mg/dL or milligrams
per deciliter. In most of the rest of the world the standard is mmol/L
or millimoles/liter. To convert from one to the other divide the value
in mg/dL by 18. So if the blood sugar level is 90 mg/dl in the United
States it is 5.0 mmol/l in Great Britain (90 divided by 18). Blood
sugar meters are coded based on the country of origin, although an
occasional patient may change from one set of units to another by
mistake, and become confused. The meter below reads 159 mg/dL (or 8.8
mmol/L). Because the author is from the United States, all blood sugar
levels in this article will be presented first as mg/dl, followed by
mmol/L). Another test, called the hemoglobin A1c or HbA1c is measured
once every three months to determine the average blood sugar levels over
the past three months. The units of HbA1c are universal.
 |
| Testing with blood glucose meter throughout the day can help with the balancing act of keeping your blood sugar in the desired range . |
The
desired range of blood sugar levels is a blood sugar in the mornings
and before meals is between 80 – 130 mg/dL (4.4 - 7.22 mmol/L). This is
slightly higher than the blood sugar level in a nondiabetic person, but
it is set a bit higher to help avoid low blood sugar reactions. Low
blood sugar reactions occur when the blood sugar falls below 70 mg/dl
(3.9 mmol/L). The first symptoms of a low blood sugar reaction are
often feeling shaky, hungry, sweaty, and jittery. If some (15 – 30 gm)
rapid acting carbohydrate (4 - 8 ounces [12 - 24 ml]) of juice or
regular soda, or 3 – 6 glucose tablets) is not consumed, the blood sugar
level can fall too low which can cause the person with diabetes to
black out (lose consciousness). Therefore all people with type 1
diabetes should test their blood sugar levels throughout the day to be
sure they are not falling too low. They should also carry a form of
rapid acting carbohydrate with them at all times in case a low blood
sugar reaction occurs (this is discussed in more detail below).
Two hours after eating the blood sugar level should be less than 180
mg/dL (10 mmol/L) and if possible, slightly lower is better - someone
without diabetes has an after eating blood sugar level of less than 140
mg/dL (7.8 mmol/L). Finally, the HbA1c level (the 3 month blood sugar
average) should be less than 7%. The normal range for the HbA1c is 4 –
6% so ideally the HbA1c should be in the normal range. However, the
problem with trying to keep blood sugar levels normal is that the risk
of low blood sugar reactions increases. So treating type 1 diabetes is
always a balancing act of trying to keep blood sugar levels from being
too high or too low.
If blood sugar levels are too high
over time, the complications of diabetes can develop. These include
diabetic eye disease (retinopathy), kidney disease (nephropathy) and
nerve damage (neuropathy). These complications are the same in people
with both type 1 and type 2 diabetes, and are discussed in more detail
in the chapter on type 2 diabetes.
As with type 2 diabetes, achieving and maintaining near normal blood
sugar levels can help prevent the development of these complications, or
delay their progression if complications already exist.
How are blood sugar levels tested?
Meters
are the devices used to test your blood sugar level and new ones are
coming out all the time. The newer meters are smaller, faster, take
smaller drops of blood, and do not require coding (which means entering
the lot number of the strips into the meter each time a new vial of
strips is used). Some of them have self-contained strips, others have
memories that store information about insulin doses and lifestyle, or
alarms that provide reminders to test blood sugar levels. Meters
themselves are not expensive, and can often be obtained for free. It is
the strips for testing blood sugar levels that are costly. This is
usually covered if you have insurance.
Having an
accurate meter is important. A blood glucose meter can be brought in
and compared to a blood sample in the doctor’s office. Meters also have
calibration solutions that test to be sure the meter is functioning
correctly. It is important to keep the meter clean and use strips that
are not expired and kept in the closed container they are provided in.
The strips are the most fragile part of the system, and exposure to air
or heat can change their accuracy.
To test the blood sugar level a test strip is inserted into the blood sugar testing meter. Then a lancing (pricking) device is used to poke the finger and obtain a small drop of blood. The drop of blood is brought to the strip (or the strip/meter is held up to the drop of blood) and the appropriate part of the strip is brought into contact with the blood. Some blood is automatically drawn up into the strip and the chemical reaction between the blood and the solution on the strip produces a signal that the meter reads as a blood sugar level. This level is displayed on the screen in 5 – 30 seconds. Each meter works slightly differently, and all come with complete instructions that should be reviewed.
Some individuals prefer forearm
(instead of fingertip) testing. Forearm testing is only accurate if
blood sugar levels are stable, that is not rising or falling.
Unfortunately, it is hard to tell if blood sugar levels are rising or
falling before choosing to poke the forearm or a fingertip. This can
lead to falsely high blood sugar readings and low blood sugar
reactions. So if in doubt, use your fingertips.
How Are Insulin Doses Determined?
As mentioned above, intensive insulin therapy requires a basal insulin
dose. This can either be given through an insulin pump (described
below) or by giving an injection of long-acting glargine insulin or
detemir insulin. The glargine insulin is usually given once a day, in
the morning or the evening. Some people need to take it twice a day,
but most of the time it is a once a day insulin. Detemir is often given
twice a day, but can also be given once a day in some people. The dose
of glargine or detemir will be determined by the physician, and will be
roughly equal to half of the total daily dose of insulin. Lean
patients with type 1 diabetes generally have a dose that is somewhere
between 10 and 20 units, although the dose can vary and needs to be
determined individually. For the insulin pump, a basal rate or basal
rates are determined by your healthcare team. This is generally between
0.6 to 1.5 units of insulin per hour and this is what the pump is
programmed to give you, day in and day out.
In addition to
the basal rate insulin, a faster acting insulin is needed before eating
and if the blood sugar level happens to be high. The premeal insulin
doses are always based on two components. The first part is a
calculation based on how much carbohydrate is going to be eaten since
the carbohydrate component of the meal is the part that increases the
blood sugar level (see nutrition section below). The calculation is
either based on grams of carbohydrate or following the exchange system
where 1 unit of rapid acting insulin = 15 grams of carbohydrate (see
below). Carbohydrate counting is one of the hardest parts of diabetes
management to do well, and yet if done correctly it makes a big
difference in control of the blood sugar levels. The best way to learn
this skill is to work with a dietitian who can teach you how to do it.
Additionally, having a book that lists a variety of foods and their
carbohydrate content is helpful. Finally, weighing and measuring food
for the first month can be useful because it trains your “carb” counting
brain. After a month of working at carbohydrate counting it becomes
second nature.Once you determine the amount of carbohydrate in the meal, you determine your dose of insulin. This ratio, called the carb ratio, is adjusted for each person, but often begins with one unit of rapid acting insulin (lispro, aspart, or glulisine given through the pump or by injection) for every 15 grams of carbohydrate (or 1 exchange). For example if two 15 gram pieces of bread are to be eaten, two units of insulin would be taken before the meal.
The second part of the equation
is a correction factor for the level of blood sugar level before
eating. So if the blood sugar level is too low less insulin is given
and if it is too high more insulin is given. A target level blood sugar
is chosen, say 100 mg/dL (5.6 mmol/L). If one unit of insulin drops
the blood sugar level 50 mg/dL (2.8 mmol/L), then the correction factor
is 50 (2.8). So if the blood sugar level is 250 mg/dL (13.9 mmol/L), 3
extra units (150 mg/dL divided by 50 or 8.3 mmol/L divided by 2.8) are
given to correct it down to 100 mg/dL (5.6 mmol/L). Now this doesn’t
always work perfectly, but as you can see adjusting your insulin like
this lets you account for changes in your diet and your blood sugar
levels.
Adjustments are also made for exercise. When
exercising insulin is used more efficiently in the body and less needed
(except in certain circumstances, discussed below). Therefore, the
insulin dose may be reduced for the meal before exercise, to avoid a low
blood sugar reaction. Sometimes less insulin is given after you
exercise, as well. The best way to determine the insulin needs for
exercise is to carefully track blood sugar levels before and after
exercise for a few days, and then work with your diabetes health care
team to figure out what your insulin doses should be.
There
are several books devoted to teaching insulin dose adjustment for
individuals on multiple injection regimens and insulin pumps. These
books include: Using Insulin, Pumping Insulin and Taking Control of Your Diabetes, Third Edition.
These books go through the theory and practical use of intensive
insulin regimens and include worksheets on insulin dosing. Although
these books can be helpful, everyone should have an individual teacher.
In addition, in larger cities look for diabetes support groups. A
general diabetes support group, where most of the patients will have
type 2 diabetes and be on pills may not be all that helpful. Try to
find a support group for people on insulin pumps, or younger individuals
with type 1 diabetes. It often helps to learn from others.
Diabetes camps
are another good way to meet and make friends with other children or
teens facing a similar challenge. These camps also provide educational
programs on diabetes management. Some camps are family oriented and
others give the parents a vacation from the daily demands of diabetes.
There are even “diabetes boot camps” for adults.
The best
way to communicate the responses of your body to insulin, food and
exercise, is to keep careful track of the information to review with
your diabetes team. Although it is something of an annoyance to keep
detailed log sheets, these are the key to evaluating whether or not your
insulin regimen is effective. After the initial set of adjustments to
figure out the correct ratios and basal insulin doses, it often suffices
to log data for a week or two before each appointment with your
diabetes team. Ask how much information is needed and how best to share
the data (email, mail, FAX or in-person).
Hypoglycemia
Hypoglycemia
is defined as a blood sugar level that is below 70 mg/dL (3.9 mmol/L).
As described above, it is associated with the symptoms of being weak,
shaky, hungry, sweaty, or having a rapid heart beat that goes away with
eating some form of rapid acting carbohydrate. This sounds simple
enough, but sometimes the warning signs of hypoglycemia aren’t noticed
and a loss of consciousness can occur. The common warning signs of
hypoglycemia are the “adrenergic” symptoms — the weak, shaky, sweaty
feelings, which are signs that your body has released catecholamines
(norepinephrine and epinephrine) into the blood stream to help raise the
blood sugar level. If these adrenergic symptoms are lost, either
because diabetes has existed for a long time (which can cause what is
called an autonomic neuropathy, meaning the body loses the ability to
react to low blood sugars) or because low blood sugar levels happen too
often (causing an abnormal adaptation to low blood sugar levels),
patients only have the neuroglycopenic symptoms, which is when the blood
sugar level falls below a certain level and the brain stops working
correctly. This means that instead of having a warning sign a person
will become confused, start slurring words, and may have a seizure or
sink into a coma. This is all because the brain uses sugar as its sole
source of fuel. These serious low blood sugar events (called severe
hypoglycemic reactions) usually require the help of someone else to
recover from them, either by injecting glucagon or calling 911 in the US
or the equivalent emergency help phone number in your country.
It is important to avoid these severe reactions, especially when
driving a car. Fortunately, most people with type 1 diabetes only have
one or two severe episodes in their lifetime, although some have them
more frequently and need careful treatment to prevent them from
happening. This is different from the less serious, easily recognized
and treated mild hypoglycemic reactions which generally occur several
times per week in well-controlled individuals with type 1 diabetes.
 |
| The new continuous glucose monitors help to fill in the picture in between standard meter readings. |
How is hypoglycemia treated?
Treating mild hypoglycemia is something of an art. Most people hate the feeling of having a low blood sugar reaction and want to use it as an excuse to eat the food they have learned to avoid, like candy, soda, and cake. But if a low blood sugar is treated with too much sugar, glucose levels will skyrocket up again and then a situation can develop in which blood sugars yo-yo up and down and up again.
To avoid
overtreating low blood sugar reactions follow the rule of 15. If the
blood sugar is below 70 mg/dL (3.9 mmol/L) and above 50 mg/dL (2.8
mmol/L), eat 15 grams of fast acting carbohydrate (see suggestions
below), wait 15 minutes, and recheck the blood sugar. If it is above 70
mg/dL (3.9 mmol/L) the hypoglycemic reaction is being treated. If the
blood sugar is not increasing, eat 15 additional grams of carbohydrate
and continue following the steps, until the blood sugar level is above
70 mg/dL (3.9 mmol/L). If the starting blood sugar is below 50 mg/dL
(2.8 mmol/L), eat 30 grams of carbohydrate and follow the steps above,
eating 30 grams of carbohydrate instead of 15 grams. Examples of 15
grams of simple carbohydrate are: three glucose tablets, 1/2 cup (four
ounces or 12 ml of juice), 1/2 can sugary soda, six Lifesavers, one cup
(eight ounces or 24 ml) milk, two tablespoonfuls (3 ml) of table sugar,
one tube of glucose gel. It is very important that all people with type
1 diabetes carry simple carbohydrate with them at all times!
After treating a low blood sugar reaction, eat a snack or a meal
containing fat, protein and carbohydrate within half an hour. This to
ensure that the blood sugar level stays in the normal range; otherwise
the effect of the simple carbohydrate, which raises the blood sugar
quickly, can wear off and the blood sugar level may drop again.
If a person with type 1 diabetes has a severe reaction and can’t eat or
drink a simple carbohydrate, then a family member or friend can give an
injection of glucagon. Glucagon is sort of an anti-insulin and raises
the blood sugar level fairly rapidly. However, people often forget to
keep glucagon on hand (it must be prescribed by a physician and expires
every six to 12 months). Also, the friend/relative of the person with
diabetes needs to be able to administer the injection. Instructions are
provided on the glucagon kit, but it helps to have practiced mixing up
the glucagon once before it has to be given in an emergency.
If glucagon isn’t available, call 911 in the US or the equivalent
emergency phone number. The paramedics have glucagon, as well as sugar
to give by vein, so they can easily help raise the blood sugar level.
No one should try to force a person with type 1 diabetes to drink juice
or eat sugar, especially if the person is unconscious. This could
result in juice being inhaled into the lungs, and that can cause serious
problems. Overall, although frightening and upsetting, these severe
reactions are treatable. It is important to contact your diabetes team
if one happens so they can help adjust your insulin (less insulin is
often needed the next day) and work on preventing another episode.
Because a reaction could occur when you are alone, it is very important
that you wear a medical alert bracelet. There are many companies who
make medical alert products. Some of these are: MedicAlert, American Medical-ID, Medic-ID, and ID-Tags.com. Some websites make nontraditional-looking medical alerts that are particularly good for children. Some examples are: MediCharms and Lauren'sHope. At the Children With Diabetes website a fairly complete listing of all of the medical alert providers is available.
What is carbohydrate counting and how is it done?
Counting carbohydrates is the key to success when living with type 1
diabetes. All people with type 1 diabetes do this, whether it is
conscious or unconscious. Because giving insulin shots mimics the role
of a pancreas, and a pancreas gives insulin based on how much
carbohydrate is eaten, there is no way to ignore the carbohydrate
content of the meal. Some people, with fixed regimens of insulin
(meaning the dose doesn’t vary much on a day to day basis) eat the same
amount of carbohydrate for each meal. Obviously this requires some
planning to have the right amount of carbohydrate in each meal. Others,
on the more flexible regimens, such as multiple daily injections and
insulin pumps, need to determine how many carbohydrates they want to
eat, and then adjust the insulin dose accordingly.
To
learn how to count carbohydrates accurately, make a study of it. It
takes several months of practicing to get good at it. The best way to
start learning about carbohydrate counting is to meet with a registered
dietitian who is an expert in diabetes. Additionally, there are books
and websites that can help. A few of these are: Complete Guide to Carb Counting, 2nd Edition, Barbara Kraus' Calories and Carbohydrates, and The CalorieKing.
Eating isn’t just about understanding carbohydrates (although carbs
have the most immediate effect on blood sugar levels). An overall
well-balanced diet is important, as well. Just as for all people, eat
healthy, unprocessed foods that are in high in fiber, vitamins, and high
quality nutrients. Limit the amount of saturated fat, trans fat and
cholesterol in your diet. Eat high quality lean protein in moderate
amounts. Each individual has their own best diet, and the dietitian can
help develop the overall meal plan.
What is a carbohydrate?
A
carbohydrate means the portion of the diet that breaks down readily to
sugar in the blood stream. Simple, refined sugars like table sugar are
absorbed quickly into the blood stream and raise glucose levels. More
complex sugars have to be broken down before they are absorbed, and are
often called starches, like pasta and rice and bread and potatoes. This
simply translates to all foods that are white, since with the exception
of egg whites and some types of fat, most white foods are sugars and
starches, and will raise blood sugar levels if eaten. Fruits,
vegetables and milk are also sources of carbohydrate. The goal of
creating a diet for each person with type 1 diabetes, is to incorporate
the foods you like to eat, in appropriate quantities, and to give the
necessary amount of insulin to cover the blood sugar rise following that
meal.
What is needed to learn carbohydrate counting?
In addition to a dietitian, three tools are: 1) a good guide listing
the carbohydrate content of foods, 2) a food measuring scale, and 3) a
set of measuring cups and spoons. Assemble the tools and start making
simple meals, measuring the grams of carbohydrate and giving insulin as
directed by your health care team. Doing this will build knowledge, and
eventually estimating the carbohydrate content of a meal will become
second nature.
Reading food labels
For prepared food the amount of carbohydrate in each serving is on the
label on the food container. In addition to noting the total number of
carbohydrate grams in a food, it is very important to note what the
designated serving size is. It is surprising how small a serving size
can be, and if more than one portion of food is to be eaten the
carbohydrate content needs to be proportionally increased.
A standard US food label found on many packaged foods.
What is the glycemic index?
The
glycemic index is a way of comparing one type of carbohydrate to
another carbohydrate. Although all carbohydrate raises blood sugar
levels, some types of carbohydrate raise your blood sugar levels more
than others. To study this researchers gave people with type 1 diabetes
a piece of white bread and measured how high it made the blood sugar
level go up after it was eaten. Based on that, the blood sugar response
to bread is set at 100. Other carbohydrates are compared to the
response to the bread. If another carbohydrate doesn’t make the blood
sugar go up as high as the bread it, it is said to have a lower glycemic
index. Carbohydrates that cause very little increase in blood sugar,
such as lentils, which have a glycemic index of 29, are considered low
glycemic index foods. When eating these foods less insulin may be
required for the same total amount of carbohydrate. Your dietitian can
teach you about adjusting for lower glycemic index foods. Some
recommend subtracting one unit of insulin for each five grams of fiber
eaten.
What are the effects of exercise?
People with type 1 diabetes have the same motivation to exercise as do
people without diabetes. Exercise helps maintain lean body mass and
fight the effects of aging. It helps lower rates of heart disease,
cancer, obesity, and osteoporosis. It also provides a sense of
well-being and helps with appearance. Exercise increases strength and
flexibility. It improves the fat in the blood stream, lowering
triglycerides, and increasing the HDL (good) cholesterol in the blood.
It helps fight stress and even improves sleep. Most people should
exercise five days a week for at least 30 minutes at a time and, ideally
up to one hour for each session.
Before starting an exercise program, check with your diabetes healthcare provider. If you are over 40 years of age you may need to have your heart checked before starting to exercise. If you have had diabetic eye damage your ophthalmologist should guide you as to what types of exercise are appropriate. People with nerve damage to their feet, especially if they have had foot ulcers and/or amputations should contact their podiatrist or other foot care provider to get advice on what shoes to wear and what kind of exercise is best. Finally, adjustments in insulin and carbohydrate intake will need to be made to avoid low blood sugar reactions since exercise improves sensitivity to injected insulin. A good resource is “The Diabetic Athlete” by Sheri Colberg and the Diabetes Exercise and Sport Association.
The best time to exercise is 90 minutes after eating. This is when the
rapid acting insulin is leaving the body and there is a good level of
sugar in the blood. If exercise will be moderate to strenuous the
premeal dose of insulin for the meal eaten before exercise may need to
be reduced. In addition, exercise during the day can lead to an
increase in insulin sensitivity overnight and some people need to
decrease their dose of basal or long acting insulin on the days they
exercise, or eat a bedtime snack to prevent low blood sugar levels while
they are sleeping. To learn how to make adjustments for exercise,
testing the blood sugar level before and after (and sometimes during)
exercise helps determine insulin doses and carbohydrate requirements.
The response to exercise may also change over time; usually exercise
lowers blood sugar levels, but when just starting out or performing very
intensive exercise, blood sugar levels can go up when stress hormones
(epinephrine and norepinephrine) are released.
Tools for Injecting Insulin
Although diabetes is not yet curable, the tools for managing diabetes
are becoming more and more refined. Simple advances can make a big
difference. For instance, insulin syringes come in a variety of
sizes—some hold only 30 units and have half-unit increments to make
measuring small doses easier. Needles come in different sizes and
lengths—mini, short and regular. A 31 gauge needle is the smallest (the
bigger the number the smaller the needle) and may hurt the least. The
physician writing the prescription for the needles (whether syringes
with needles or pen needles [see below]) must specify the length, gauge
and type of needle desired.
Insulin Pens
Insulin pens are wonderful devices that literally look like slightly thicker pens, which contain insulin and are dosed by turning a dial. The benefit of pens is that they avoid the fuss and bother of drawing up insulin from a vial with a syringe—the prefilled pens are ready to go. Some pens are completely disposable and others have replaceable cartridges. Either way, once a pen needle is screwed on the top of the insulin pen cartridge it is ready to use. With all pens the needle must be first flushed with insulin each time it is used to achieve an accurate dose. To flush the pen needle, dial up four to five units and push the plunger down and watch to see that insulin is flowing out the end of the needle. The pen is now ready to use. Pens are used very commonly in Europe and fairly rarely in the United States, largely due to differences in payment by insurance plans. With time, however, pen use is increasingly covered in the United States are more people are using them.
The steps for a proper injection are simple. Dial up the desired dose, insert the needle into the skin, push the plunger down and then wait for five seconds after the insulin is injected before removing it from the skin. These pens are easy to carry in a purse or backpack and are helpful when giving insulin injections before each meal. The down side to pens is that insulins can’t be self mixed (meaning mixed together by the patient) (although prefilled pens with insulin mixtures exist). Pens also have a limit to how much insulin can be given in one dose, often around 60 units. Finally, pens are often not covered by insurance companies because they are considered a convenience item, although being more convenient can hopefully translate to better control.
Insulin Pumps
Insulin pump therapy is another way of giving insulin, and is effective
for many people with type 1 diabetes. However, many individuals can
achieve good blood sugar control giving injections of insulin before
meals and a once or twice a day injection of basal insulin. There is no
one way to give insulin, and some people may prefer injections for a
few years and then switch to a pump or vice versa. The goal is to
safely and consistently bring blood sugar levels to normal and keep the
HbA1c below 7% without severe hypoglycemia. No matter which approach is
chosen it requires work and frequent blood sugar testing to make sure
that appropriate insulin doses are given.
An insulin pump is a
mechanical device, about the size of a pager, which provides a constant
flow of rapid acting insulin through a catheter that is inserted under
the skin. This catheter is inserted every two to three days with an
inserter that helps guide its placement. The catheter is connected to
the pump, which contains the insulin. The official title for this
therapy is “continuous subcutaneous insulin infusion” or CSII therapy.
Several companies make insulin pumps: Animas, MiniMed, Deltec, Accu-Chek, OmniPod.
 |
| Medtronic MiniMed Paradigm® REAL-Time System - Courtesy Medtronic, Inc. |
A pump does NOT measure your blood sugar levels – you still have to prick your finger for that – but continuous glucose monitoring devices are being developed and blood sugar levels can be displayed on the MiniMed Paradigm pump’s LCD screen. The pump is filled with rapid acting insulin (lispro, aspart, glulisine) and it gives a slow little trickle of insulin based on a basal rate that is calculated by your diabetes healthcare team. Before each meal or snack information is entered into the pump consisting of the blood sugar level and the amount of carbohydrate to be eaten. The pump then calculates how much insulin to given, based on the preprogrammed carbohydrate and correction ratios. It asks the user if the user agrees with the dose and, if yes, the new dose is delivered. The user can always override the pump’s recommendations and give a different dose.
In some ways the pump
is much more convenient than shots—the insulin is ready to give, right
in the pump. But there are several things that make this system
difficult. For one thing the pump has to be worn somewhere on your
body. Men tend to wear it on their belts; women will often hide it in
their bra. At night the pump is worn on boxer shorts or a pajama top
with a pocket. The tubing is also a part of the device and must be kept
free of kinks and clogging, although the Omnipod pump attaches directly
to the body and does not require tubing. Finally, the flow of insulin
from the pump into the body is easily disrupted. If this happens for
too long a condition diabetic ketoacidosis (DKA) can develop.
Therefore, the blood sugar level must be tested at least four times a
day. If it becomes high for no reason then insulin should be given by
injection and the pump infusion site changed.
There are many benefits to using an insulin pump. Unlike long acting insulin shots, which provide a fairly constant amount of insulin, the pump allows very small changes in the basal rate to be made in order to cover changing insulin needs during the day and particularly overnight. It is also easily turned off—it can be suspended or the basal rate reduced during exercise or if blood sugar levels drop too low. The newer pumps make it easier to do the complex calculations of carbohydrate and correction doses, as well as a calculation to tell you how much insulin is still acting in the body from the last insulin dose. Insulin doses from a pump can also be given in tenths of units, which is more precise than when given with an injection.
Continuous Glucose Monitoring Devices
Although methods for measuring blood sugar levels without finger pricks
do not yet exist, continuous glucose monitoring (CGM) is a technique
that has become increasingly helpful in the management of type 1
diabetes. These devices consist of a sensor that is inserted under the
skin (the sensor is about the size of a small piece of stiff fishing
line or the bristle in a hairbrush), and a transmitter that attaches to
the sensor and sends an infrared signal to the receiver. The receiver is
a pager-like device that can be worn on a belt or kept in a purse and
provides continuous information on glucose levels. Unlike many insulin
pumps, no tubing is involved. These sensors monitor the interstitial
(meaning the clear fluid just under the skin, not blood, although they
are calibrated as though they are reading a blood sugar level) sugar
levels every one to five minutes. Each sensor lasts from three to seven
days. The devices can be set to alarm if the blood sugar level is too
high or too low, but perhaps more importantly they can alarm if the
blood sugar level is falling or rising too quickly so that high and low
blood sugar levels can be avoided. For instance, if the blood sugar
level before a meal is 100 mg/dL (5.6 mmol/L) and falling quickly a
much smaller dose of insulin should be given than if the blood sugar is
100 mg/dL (5.6 mmol/L) and rising rapidly.
Adjusting to all
of this new information is one of the concerns about using continuous
monitors. It could be dangerous if insulin is given every few minutes
because the blood sugar level is high, instead of giving insulin once
and then waiting for two to three hours for a response. Giving too much
insulin too often is dangerous. On the other hand, the added benefit
of being alerted to rising and falling blood sugar levels is very
helpful, and with training continuous glucose monitoring can be used
safely. The two sensors that are available are through Minimed (both with their pump and well as without) and Dexcom.
What is Symlin?
Symlin
(generic name: pramlintide) is structurally similar to a hormone called
amylin that is released from the beta-cells in the pancreas along with
insulin. In people with type 1 diabetes not only is the body producing
no insulin, but amylin production is deficient. Although amylin itself
can’t be injected because it forms clumps, a similar compound,
pramlintide can be given. What pramlintide does is to slow the
absorption of food (which is too rapid in most people with type 1
diabetes), lowers the after eating levels of glucagon (a hormone that
increases blood sugar levels), and reduces appetite. Thus Symlin can
lower blood sugar levels and weight if given before meals in patients
with type 1 diabetes.
Symlin is available in both
vials and in pens. The main side effect with Symlin is nausea and
sometimes vomiting. These side effects are reduced if a low dose is
used initially and gradually increased. It is given along with the
premeal insulin, although the insulin dose given before needs to be cut
in half when the Symlin is started in order to avoid low blood sugar
reactions. (If the Symlin leads to a decrease in appetite it would be
dangerous to give the usual dose of insulin and then end up eating
less). The specific recommendations for starting Symlin should be given
by the health care provider. Successful use of Symlin leads to a
reduction in the HbA1c level, a lower premeal insulin dose requirement
and some weight loss. People who shouldn’t use Symlin include those
with a gastroparesis (a condition whereby stomach emptying is too slow)
and patients who have out of control blood sugar levels.
| Researcher working at the Larry L. Hillblom Islet Research Center located at UCLA. |
Will there be a cure for type 1 diabetes?
The
best way to cure type 1 diabetes would be to find a way to turn off the
immune system so that it stops destroying the beta-cells. Researchers
are working hard to find a way to do this. Early studies have shown
some improvement, but turning off the immune system is a tricky business
because if done too much it can cause immune deficiency (for example
HIV/AIDS).
Another approach is to give more beta-cells (in the
form of islet cells), in the hopes that they will replace the missing
beta-cells. These islet cell transplants have been done at selected
centers in the United States and Canada, but there are several problems
with this procedure. First, it requires many islet cells and often
donations from two or more pancreases. Organ donations are limited,
making islet cells in short supply. Second, the person getting the
islet cells will destroy them (because they have type 1 diabetes) so
immunosuppressive drugs need to be given. These drugs have many side
effects and for many the side effects are worse than giving insulin
injections. Finally, over time the transplants fail and insulin use is
required again. So this is not a permanent solution.
Researchers are working on ways to overcome some of the barriers found
with islet cell transplantation. Stem cells may provide a good source
for islet cells. Certain cells in the body, such as liver cells, may be
transformable into islet cells so person could be their own source of
new islet cells. Encapsulation techniques are being researched so that
islet cells could be covered in a capsule that prevents them from being
destroyed but still allows them to function. Finally, newer and safer
immunosuppressive drugs are being developed.
Many organizations, such as the American Diabetes Association and the Juvenile Diabetes Research Foundation are working towards a cure for type 1 diabetes. TrialNet is an international group of researchers who conduct research studies to help prevent and treat early type 1 diabetes and DirectNet is a consortium of researchers studying approaches for treating children with type 1 diabetes. Children with Diabetes is a group that sponsors programs for children with type 1 diabetes and their website has links to many diabetes resources.
are working towards a cure for type 1 diabetes. TrialNet is an international group of researchers who conduct research studies to help prevent and treat early type 1 diabetes and DirectNet is a consortium of researchers studying approaches for treating children with type 1 diabetes. Children with Diabetes is a group that sponsors programs for children with type 1 diabetes and their website has links to many diabetes resources.
Conclusion
The
treatment of type 1 diabetes is both simple and extremely complex.
Insulin must be given from the outside to mimic what the body should be
doing from the inside. The hardest part of type 1 diabetes for many
patients is the unrelenting quality of it: each day, all day, a person
with diabetes must test their blood sugar levels and react
appropriately. Although this can become second nature, it is still an
extra step that has to be performed before every meal, snack, and
activity. Fortunately, new technologies, such as continuous glucose
monitoring and highly effective insulin analogues, are being developed
that make living with diabetes a little bit easier. The good news is
that even if there is not yet a cure, type 1 diabetes is a disease that
can be treated effectively. People with type 1 diabetes are able to
live long and healthy lives, without the development of diabetic
complications that plagued earlier generations of people who suffered
from the disease.
Appendix: The Role of Diet in Type 1 Diabetes
With Meg Werner Moreta, RD, CDE
Meg Werner Moreta counseling a patient at the USC Westside Center for Diabetes.
Types of Carbohydrates
There are five basic types of carbohydrates: starches, simple sugars,
fruits, vegetables, and dairy. Fiber and alcohol (if consumed) are also
important dietary factors. Counting carbohydrates in all these foods
is easiest when eating at home, where it is relatively simple to weigh
and measure food. In contrast, when eating at a restaurant it is hard
to know everything that is added to food that can increase blood sugar
levels. Therefore, in restaurants it is helpful to ask for foods made
simply, (e.g., grilled foods without breading or a sauce).
Starches
Starches are long chains of sugar molecules and are often the hardest
food type to measure accurately. Often one starch increases the blood
sugar level more than another in an individual patient. For example,
some find a baked potato the most difficult, while others find pasta or
rice raise the blood sugar level most dramatically.
Whatever the response to any given starch, it is important to be able to measure it. This starts by figuring out portion size for carbohydrates. A general approach is that a basic portion size is 1/2 cup (70 gm) of cooked starch (such as pasta or potatoes), with most 1/2 cup (100 gm) servings equal to 15 grams of carbohydrate. Rice is the exception because it is extremely dense, so 1/3 cup (64 gm) of rice equals 15 grams. Note: Conversion of cups to grams (volume to weight) is tricky and is dependent on the food group. The on-line calculator found at GourmetSleuth can be a useful guide.
Whatever the response to any given starch, it is important to be able to measure it. This starts by figuring out portion size for carbohydrates. A general approach is that a basic portion size is 1/2 cup (70 gm) of cooked starch (such as pasta or potatoes), with most 1/2 cup (100 gm) servings equal to 15 grams of carbohydrate. Rice is the exception because it is extremely dense, so 1/3 cup (64 gm) of rice equals 15 grams. Note: Conversion of cups to grams (volume to weight) is tricky and is dependent on the food group. The on-line calculator found at GourmetSleuth can be a useful guide.
Other
starch servings that equal 15 grams of carbohydrate are one slice of
bread or 1/2 cup (70 gm) of potatoes, beans, garbanzo beans, kidney
beans, lima beans, lentils, squashes, peas, croutons, and corn. Since
many of these starches are added to salads or meals, it helps to measure
out 15 grams worth at home, to get a feel for what it will look like
when mixed into food when dining out.
Fruits
Fruits are a good source of carbohydrate and are filled with lots of
wonderful nutrients, minerals, and vitamins. Although the sugar in
fruit can increase blood sugar levels, fresh fruit generally contains
enough fiber to blunt some of the expected increase. Cooking fruit or
mashing it to make fruit juice often increases the amount of
carbohydrate consumed, lowers the fiber content, and increases the speed
at which your blood sugar levels rise. Therefore eat fresh, uncooked
fruit as much as possible, with the exception of really dense fruit,
like bananas, that can often raise blood sugar levels too high. The
portion size for a banana is half a banana—a whole banana is two
portions, or 30 grams.
The difficulty in counting fruit
carbs is that fruit doesn’t come in prepackaged sizes. Although
sometimes fruit in the grocery store looks like it was made in a
standard mold, natural fruit often varies in size. It also varies in
ripeness, which can alter how sweet (how much simple sugar) is in the
piece of fruit. In spite of this, it would be ideal to eat 3 to 4
pieces of fruit per day.
In order to incorporate fruit
into your diet, follow these general rules: a very small apple, a small
peach, or a small pear is 15 grams of carbohydrate. Bigger ones may
need to count as 20 to 25 grams. A banana or a grapefruit is worth 30
grams. Fruit juice should be avoided, except to treat a low blood sugar
reaction. However, if fruit juice is to be consumed 4 ounces (12 ml)
is 15 grams of carbohydrate.
Fruits are a good source of carbohydrate and are filled with lots of wonderful nutrients, minerals, and vitamins.
Vegetables
Vegetables should comprise half of the calories eaten each day. In the
past non-starchy vegetables were not counted when calculating
carbohydrate grams, but if one eats enough of them, vegetables will
raise blood sugar levels because they are, in fact, carbohydrates. In
general, assume that three cups (600 gm) of non-starchy raw vegetables –
or one and one-half cups (300 gm) of cooked vegetables – equals 15
grams of carbohydrate.
Dairy Products
Dairy products often have carbohydrate, fat, and protein in them. The
label on dairy products helps determine how many grams of carbohydrate
are in a serving. For milk, eight ounces (24 ml) equals 12 to 15 grams
of carbohydrate. Typically, it is best to consume low fat dairy products
to cut back on saturated fat and cholesterol consumption.
Simple Sugars
Simple sugars (e.g., non-diet sodas, large amounts of catsup, and the
high fructose corn syrup used in many foods) increase blood sugar levels
quickly. As discussed above, 15 to 30 grams of simple carbohydrate
should be used to treat a low blood sugar reaction. Fifteen grams of
sugar can be provided by the following: two tablespoons of table sugar,
one tablespoon (1.5 ml) of honey, four ounces (12 ml) of juice, or eight
ounces (24 ml) of milk.
General Philosophy
The key is to read and study and learn the carbohydrate content of all
of the things that are eaten. One needs to be a detective and find the
hidden carbohydrate calories so the insulin can be adjusted
appropriately. The more knowledge you have, the better you’ll function
as an artificial pancreas; the better you function as a pancreas, the
more normal your blood sugar levels will be.
Another
good rule is to log your food, estimated carbohydrate content, and
insulin dose given in real day. Using your logs, you and your
healthcare team can work together to see if your blood sugar levels are
within range both before and two hours after eating. Then you can adjust
your carbohydrate ratios and correction factors if they are not
covering your carbohydrate intake adequately.
The Effects of Fiber
Fiber slows down the absorption of food. It is actually very good for
everyone, because it helps digestion function normally. More fiber
lowers the glycemic index of food and reduces how high the blood sugar
levels are after eating. Refining food means breaking down the fiber
and increasing the speed at which it is absorbed. Accounting for the
fiber in food will help further improve accuracy in carb counting. In
general if the food to be eaten contains five grams of fiber or more, it
should be subtracted from the carbohydrate total for that meal.
The Effects of Protein and Fat on Blood Sugar Levels
Protein can be converted into sugar, but this generally happens so
slowly and gradually that it doesn’t really make an obvious difference
in blood sugar levels if only three or four ounces (85 - 113 gm) are
eaten. However, if 10 ounces (283 gm) or more are eaten, extra insulin
might need to be added to account for the fact that protein can turn
into glucose in the body over time. This function of protein, the slow
increase in blood sugar levels over time, means that it can help keep
blood sugar levels in the normal range in between meals or overnight.
Fat slows gastric emptying and can prolong the effects of
food in the gastrointestinal track. Foods such as pizza, which is high
in fat and simple carbohydrate, can increase blood sugar levels
immediately after eating and then several hours later as the food is
slowly absorbed. Fat will never turn into sugar itself, but by slowing
the absorption of carbohydrate, it can also help keep blood sugar levels
higher over time.
Alcohol
Although
it seems like alcohol should be sugar in the blood, its unique form
doesn’t usually raise blood sugar levels. In fact, pure alcohol reduces
how much sugar the liver makes, and it can lower the blood sugar
level. So when drinking alcohol it is important to eat some food at the
same time, in order to avoid low blood sugar reactions. An alcoholic
drink, however, doesn’t always lower the blood sugar levels, because
drinks are sometimes combined with sweet mixers; these should be taken
into account. Beer also has more carbs than wine. In short, it is
important to learn the impact of various types of alcohol on your blood
sugar levels.
From a health-perspective, drinking a
small amount of alcohol is probably a good thing, as long as there is no
history of alcohol addiction. Too much alcohol is clearly bad – brain
and liver cells start dying – but a glass of wine with dinner may help
lower the risk of heart disease. This has been studied in people with
and without diabetes. So although people who don’t drink shouldn’t
start drinking, people who drink in moderation and who have type 1
diabetes can continue. Just keep in mind the potential for low blood
sugar reactions overnight, especially if extra alcohol is consumed. Be
sure to eat a balanced meal and test blood sugar levels to avoid running
into trouble.
Diabetes Organizations:
- American Diabetes Association: http://www.diabetes.org/
- International Diabetes Federation: http://www.idf.org/
- National Diabetes Education Program: http://ndep.nih.gov/
- American Association of Diabetes Educators: http://www.diabeteseducator.org/
- American Dietetic Association: http://www.eatright.org/
- Diabetes Exercise and Sports Association (DESA): http://www.diabetes-exercise.org/
- Juvenile Diabetes Research Foundation: http://www.jdrf.org/
- Children with Diabetes: http://www.childrenwithdiabetes.com/
- Center for Disease Control: http://www.cdc.gov/
- American Heart Association: http://www.americanheart.org/
- Comprehensive Foot Health Site: http://www.foot.com/
Patient Education Events
- Taking Control of Your Diabetes: http://www.tcoyd.org
- ADA Diabetes Expo: http://www.diabetes.org
- Green Mountain at Fox Run: http://fitwoman.com
People With Diabetes Blogs:
- Diabetes Mine by Amy Tenderich: http://www.diabetesmine.com/
- David Mendosa: http://www.mendosa.com/
- Diabetes Sisters: http://www.diabetessisters.com
Patient Education Websites
- For Your Diabetes Life: http://www.dlife.com/
- America on the Move: http://www.americaonthemove.org/
- How I Do Diabetes.com (Sponsored by Novartis): http://www.howidodiabetes.com/
- YourDiabetesGoals.com (Sponsored by Amylin): http://www.yourdiabetesgoals.com/
- Do>Groove (Sponsored by BlueCross/Blue Shield - MN): http://www.do-groove.com/
- Healthy Updates - Diabetes: http://www.healthyupdates.com/diabetes/
Anne Peters, M. D.
- USC Westside Center for Diabetes: http://www.uscdiabetes.com
- Keck Diabetes Prevention Initiative: http://www.wmkeck.org/contentManagement/PR_95271a31-9585-4508-a17c-67d8d0235b41.htm
- Peters AL. “Conquering Diabetes.” Hudson Street Press/Penguin Publications, New York City, New York, 2005. http://www.conqueringdiabetes.com/
- Dr. Anne Peters in the PBS series Remaking American Medicine "The Stealth Epidemic": http://www.remakingamericanmedicine.org/episode3.html
- Interview of Dr. Anne Peters on Diana Rehm -WAMU Audio: http://wamu.org/programs/dr/05/08/12.php
- Interview of Dr. Anne Peters on Exercising with Diabetes -Diabetes Health: http://www.diabeteshealth.com/read/2006/03/01/4528.html
- Transcript of Dr. Peters on Larry King Live: http://transcripts.cnn.com/TRANSCRIPTS/0505/20/lkl.01.html
- Today Show videos (after an opening ad): Segment 1 - Segment 2
- Close Concerns interview.
Additional Links
Official website for Indy Lights driver Charlie Kimball: http://www.charliekimball.com/
Official website of dancer Zippora Karz: http://www.zipporakarz.com/
Photographer Mark Harmel: http://www.harmelphoto.com/














