Washington: Findings suggest ways to block nerve cell damage in neurodegenerative diseases. In many neurodegenerative conditions — Parkinson’s disease,
amyotrophic lateral sclerosis (ALS) and peripheral neuropathy among them
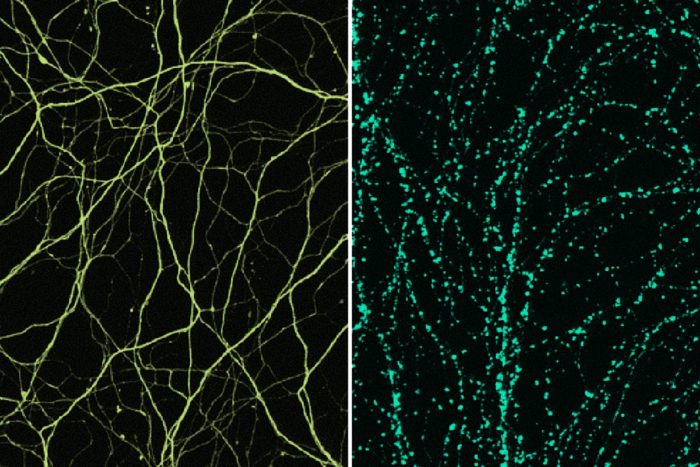
— an early defect is the loss of axons, the wiring of the nervous
system. When axons are lost, nerve cells can’t communicate as they
should, and nervous system function is impaired. In peripheral
neuropathy in particular, and perhaps other diseases, sick axons trigger
a self-destruct program.
In new research, scientists at Washington University School of
Medicine in St. Louis have implicated a specific molecule in the
self-destruction of axons. Understanding just how that damage occurs may
help researchers find a way to halt it.
The study is published March 22 in the journal Neuron.
“Axons break down in a lot of neurodegenerative diseases,” said senior author Jeffrey D. Milbrandt, MD, PhD,
the James S. McDonnell Professor and head of the Department of
Genetics. “Despite the fact these diseases have different causes, they
are all likely rooted in the same pathway that triggers axon
degeneration. If we could find a way to block the pathway, it could be
beneficial for many different kinds of patients.”
Since the molecular pathway that leads to loss of axons appears to do
more harm than good, it’s not clear what role this self-destruct
mechanism plays in normal life. But scientists suspect that if the
pathway that destroys axons could be paused or halted, it would slow or
prevent the gradual loss of nervous system function and the debilitating
symptoms that result. One such condition, peripheral neuropathy,
affects about 20 million people in the United States. It often develops
following chemotherapy or from nerve damage associated with diabetes,
and can cause persistent pain, burning, stinging, itching, numbness and
muscle weakness.
“Peripheral neuropathy is by far the most common neurodegenerative disease,” said co-author Aaron DiAntonio, MD, PhD,
the Alan A. and Edith L. Wolff Professor of Developmental Biology.
“Patients don’t die from it, but it has a huge impact on quality of
life.”
In previous studies, Stefanie Geisler, MD,
an assistant professor of neurology, working with DiAntonio and
Milbrandt, showed that blocking this axon self-destruction pathway
prevented the development of peripheral neuropathy in mice treated with
the chemotherapy agent vincristine. The hope is that if methods are
developed to block this pathway in people, then it might be possible to
slow or prevent the development of neuropathy in patients.
Toward that end, the Milbrandt and DiAntonio labs showed that a
molecule called SARM1 is a central player in the self-destruct pathway
of axons. In healthy neurons, SARM1 is present but inactive. For reasons
that are unclear, injury or disease activate SARM1, which sets off a
series of events that drains a key cellular fuel — called nicotinamide
adenine dinucleotide (NAD) — and leads to destruction of the axon.
Though the researchers previously had shown SARM1 was required for this
chain of events to play out, the details of the process were unknown.
SARM1 and similar molecules — those containing what are called TIR
domains — most often are studied in the context of immunity, where these
domains serve as scaffolds. Essentially, TIR domains provide a haven
for the assembly of molecules or proteins to perform their work.
The researchers had assumed that SARM1 acted as a scaffold to provide
support for the work of destroying axons, beginning with the rapid loss
of cellular fuel that occurs minutes after SARM1 becomes active. The
scientists set about searching for the demolition crew — the active
molecule or molecules that use the SARM1 scaffold to carry out the
demolition. The study’s first author, Kow A. Essuman, a Howard Hughes
Medical Institute Medical Research Fellow and an MD/PhD student in
Milbrandt’s lab, performed a litany of cellular and biochemical
experiments searching for the demolition crew and came up empty.
“We performed multiple experiments but could not identify molecules that are traditionally known to consume NAD,” Essuman said.
But as a last resort, the investigators tested SARM1 itself. To their
great surprise, they found it was doing more than simply providing a
passive platform. Specifically, the researchers showed SARM1’s TIR
domain acts as an enzyme, a molecule that carries out biochemical
reactions, in this case destroying axons by first burning all their NAD
cellular fuel.
“There are more than 1,000 papers describing the function of proteins
containing TIR domains,” DiAntonio said. “No one had ever shown that
this type of molecule could be an enzyme. So we went into our
experiments assuming SARM1 was only a scaffold and that there must be
some other enzyme responsible for demolition of the axon. We essentially
searched for a demolition crew, only to discover that the scaffold
itself is destroying the structure. It’s the last thing you would
expect.”
The findings suggest molecules similar to SARM1 — those with TIR
domains and known to serve as scaffolds in the immune system — may prove
to have additional functions that go beyond their structural roles. The
research also invites a search for drugs that block the SARM1 enzyme
from triggering axonal destruction.