St Louis: Inflammation is one of the main reasons why people with diabetes
experience heart attacks, strokes, kidney problems and other, related
complications. Now, in a surprise finding, researchers at Washington
University School of Medicine in St. Louis have identified a possible
trigger of chronic inflammation. Too much fat in the diet promotes insulin resistance by spurring
chronic inflammation. But the researchers discovered, in mice, that when
certain immune cells can’t manufacture fat, the mice don’t develop
diabetes and inflammation, even when consuming a high-fat diet.
The study is available Nov. 2 as an advance online publication from the journal Nature.
“The number of people with diabetes has quadrupled worldwide over the
last 20 years,” said senior investigator Clay F. Semenkovich, the Irene
E. and Michael M. Karl Professor and director of the Division of
Endocrinology, Metabolism & Lipid Research at the School of
Medicine. “We have made modest progress in making it less likely for
some people with diabetes to have heart attacks and strokes. However,
those receiving optimal therapy are still much more likely to die from
complications driven by chronic inflammation that is, at least in part,
generated by these immune cells.
“But by blocking the production of fat inside these cells, it may be
possible to prevent inflammation in people with diabetes and even in
other conditions, such as arthritis and cancer, in which chronic
inflammation plays a role. This could have a profound impact on health.”
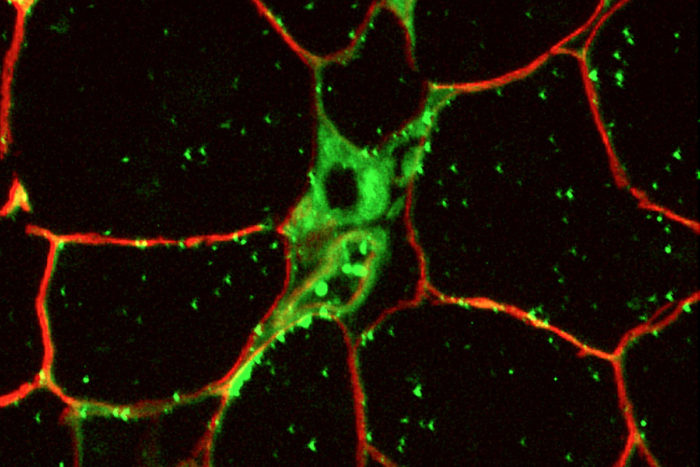
Semenkovich’s team made genetically altered mice that could not make
the enzyme for fatty acid synthase (FAS) in immune cells called
macrophages. Without the enzyme, it was impossible for the mice to
synthesize fatty acids, a normal part of cell metabolism.
“We were surprised to find that the mice were protected from
diet-induced diabetes,” said first author Xiaochao Wei, PhD, an
instructor of medicine. “They did not develop the insulin resistance and
diabetes that normally would have been induced by a high-fat diet.”
Through a series of experiments in the animals and in cell cultures,
the researchers, including Douglas F. Covey, PhD, a professor of
developmental biology and biochemistry, and Daniel S. Ory, MD, a
professor of medicine and of cell biology and physiology, found that if
macrophages could not synthesize fat from within, the external membranes
of those cells could not respond to fat from outside the cells. That
prevented the cells from contributing to inflammation.
But eliminating inflammation altogether is not the answer to
preventing diabetic complications because inflammation is also vital for
clearing infectious pathogens from the body and helps wounds heal.
Still, Semenkovich said the new findings may have profound clinical
implications.
“An inhibitor of fatty acid synthase actually is now in clinical
trials as a potential cancer treatment,” he explained. “And other drugs
have been developed to inhibit fatty acid synthase in diabetes, too. One
possibility that our work suggests is that altering the lipid content
in the cell membrane may help block cancer metastases and complications
of diabetes.”
Drugs currently in use to block fatty acid synthase, as well as other
developing strategies, potentially could allow for chronic inflammation
to be blocked, without completely eliminating the ability of
macrophages to fight infection.
The researchers also plan to take a look at existing drug compounds
that change the lipid composition in cells. Such medications failed in
clinical trials, but they may have an effect on the membranes of
macrophages and therefore may lower the risk of diabetes complications,
Semenkovich said.