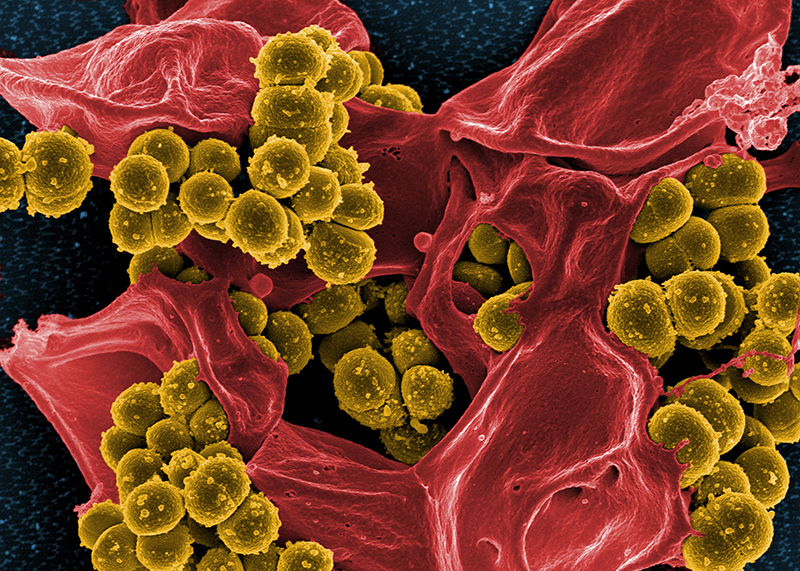
Harvard: Infections of the skin or other soft tissues by the hard-to-treat MRSA (methicillin-resistant Staphylococcus aureus) bacteria appear to permanently compromise the lymphatic system, which is crucial to immune system function. In a report published online in Science Translational Medicine,
Harvard Medical School investigators based at Massachusetts General
Hospital describe findings that MRSA infection impairs the ability of
lymphatic vessels to pump lymphatic fluid to lymph nodes in mouse
models, which may contribute to the frequent recurrences of MRSA
infection experienced by patients.
“We found that MRSA produces toxins that kill the muscle cells critical to the pumping of lymph,” said senior study author Timothy Padera, HMS associate professor of radiation oncology at Mass General.
“MRSA with a genetic deficiency that lowers the amount of toxin
produced does not kill lymphatic muscle cells, which both supports the
role for bacterial toxins in the post-MRSA impairment of lymphatic
function and may also suggest a possible treatment strategy,” he added.
Serious skin infections called cellulitis are reported in about 14
million U.S. patients annually, with as many as 30 percent caused by
MRSA. Serious cases requiring intravenous antibiotics lead to 500,000
hospitalizations each year, and 50,000 of those patients will have
recurrent infections that require hospital readmission within a month.
Patients with lymphedema—swelling and fluid buildup caused by damage
to or blockage of the lymphatic system—are particularly prone to
recurrent infections, which can exacerbate existing lymphedema. But
until now, no studies have investigated the potential interactions
between bacterial infections and lymphatic function.
In contrast to the cardiovascular system, in which blood is propelled
through arteries and veins by the pumping of the heart, in the
lymphatic system, lymphatic fluid—which carries immune cells and other
important factors—is pumped along by the contraction of the lymphatic
vessels, driven by lymphatic muscle cells.
Persistent Impairment
Experiments in mouse models of MRSA tissue infections revealed that
the infection itself cleared within 30 days and associated inflammation
was gone within 60 days. But the lymphatic vessels in MRSA-infected
tissues showed abnormalities, including increased vessel diameter and
weaker, less frequent contractions, that were still present 120 days
after the induction of infection.
Close examination revealed that the number of lymphatic muscle cells
surrounding lymphatic vessels was depleted as late as 260 days after
infection.
“We had assumed that we would find results similar to our previous
measures of impaired lymphatic function in inflammation that was not
associated with an infection,” Padera said. “But while lymph pumping was
restored after the resolution of sterile inflammation, MRSA-induced
impairment persisted long after the infection was resolved and the
inflammation had stopped.”
“This persistence long after bacteria have been cleared can be explained by the loss of lymphatic muscle cells,” he said.
Exposure of cultured mouse and human lymphatic or smooth muscle cells
to the proteins produced by MRSA led to the death of these cells, and
detailed analysis of MRSA-produced proteins identified a significant
number of known pathogenic toxins.
Since expression of many MRSA toxins is controlled by a genetic element called the accessory gene regulator (agr), the team tested a mutant form of MRSA lacking the agr against several types of cultured cells and in their animal model.
The agr-mutant MRSA did not produce the muscle cell-killing
proteins, and lymphatic function—including the strength and frequency of
vessel contraction—was significantly better in mice infected with the
mutant strain than in animals infected with a nonmutated strain.
“Our results strongly suggest that targeting the action of the agr during
and after MRSA infection may preserve lymphatic muscle cells and, as a
result, lymphatic function,” Padera said. “Now we need to confirm
whether MRSA infection leads to impaired lymphatic function in humans
and identify the specific MRSA toxins that cause the death of lymphatic
muscle cells.”
Support for the study includes National Institutes of Health grants
R21 AI097745, DP2 OD008780, R01 CA214913 and R01HL128168, along with
support from the MGH Executive Committee on Research Interim Support
Fund.