Washington: For patients with difficult-to-treat cancers, doctors increasingly
rely on genomic testing of tumors to identify errors in the DNA that
indicate a tumor can be targeted by existing therapies. But this
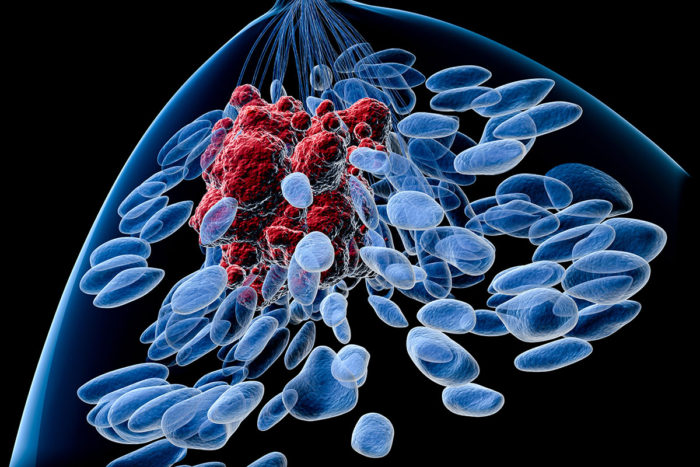
approach overlooks another potential marker — rogue proteins — that may
be driving cancer cells and also could be targeted with existing
treatments. If DNA can be described as the body’s genetic blueprint, proteins can
be thought of as the construction workers who carry out the plan.
Studying the blueprint can be vital to understanding genetic diseases,
including cancer, but that focus also means that some problems arising
with the workers may be missed.
Studying mice with breast tumors transplanted from patients,
researchers at Washington University School of Medicine in St. Louis,
The Broad Institute of MIT and Harvard, and Baylor College of Medicine
have analyzed the proteins present in these tumors. The researchers
demonstrated that some protein alterations can be used to identify drugs
that may work against some cancers. The work is part of the National
Cancer Institute’s (NCI) Clinical Proteomic Tumor Analysis Consortium
efforts.
The study is published March 28 in Nature Communications.
“Proteins carry out most of the biological functions in the cell,” said senior author Li Ding, PhD,
an associate professor of medicine at Washington University. “Knowing
the DNA sequence does not automatically tell us everything about the
proteins doing work in the cells. This is another layer of tumor
complexity that we need to explore to identify new therapies.”
Ding said recent advances in a technology called mass spectrometry
and in techniques to analyze massive quantities of data have made
complex studies of the proteins in tumor cells possible. Another reason
to prioritize the systematic study of proteins in tumors — cancer
proteomics — is that the vast majority of cancer therapies developed
from genetic studies actually target proteins.
“Identifying the rogue proteins of cancer is an important pathway
toward developing new drugs,” said co-author R. Reid Townsend, MD, PhD, a
professor of medicine and director of the Proteomics Shared Resource at
Washington University.
“We can use proteomics to confirm and validate our genomics findings,” said Ding, also an assistant director of The McDonnell Genome Institute
at Washington University School of Medicine. “In addition, it’s another
tool to uncover additional events that drive cancer and are specific to
individual patient tumors, including the amount of the ‘rogue’ protein,
its specific form, or the type and extent of chemical modifications of
the proteins that we know are treatable with approved or investigational
drugs. We also can test these therapies in the mice before we evaluate
them in patients.”
Steven A. Carr, PhD, of the Broad Institute, said the team analyzed a
chemical modification called phosphorylation, which plays a central
role in how healthy, as well as diseased, cells communicate.
“Disruption or enhancement in such signaling is often directly
related to disease mechanism and can be targeted for therapy,” Carr
said.
The researchers studied 24 tumor samples from breast cancer patients
after the samples were transplanted into mice. Twenty-two of the
transplanted samples retained their genetic and proteomic identities as
specific types of breast cancer. A proteomic analysis of the tumors also
identified multiple protein targets that have the potential to respond
to drugs.
For example, the researchers showed dialed-up activity of multiple
protein pathways that could be targeted with investigational drugs
called PI3K inhibitors and mTOR inhibitors, separately and in
combination, depending on the tumor. They also showed that drugs against
a type of breast tumor called HER2 positive breast cancer — such as the
dual ERBB2/EGFR inhibitor lapatinib — potentially could benefit more
patients than currently receive them, if analysis of the tumor proteins
is taken into consideration.
While most of these tumor models recapitulated specific types of
breast cancer, Ding said the scientists were surprised to see that two
of the 24 tumors evolved into a completely different type of cancer
after transplantation into the mice. Instead of breast cancer, they
resembled lymphoma and were driven by the cancer-causing virus
Epstein-Barr, according to the researchers. Lymphomas are cancers of
immune cells that may have arisen from lymphatic tissue present in the
breast tumors transplanted into the mice.
The analysis of the lymphoma-like cancers was the first proteomic
study of this type of tumor. Though unintentional, Ding said the
analysis provides an explanation for why investigational drugs that
inhibit a protein called BTK have been effective in treating patients
with lymphoma.
“Since it is the proteins that interact directly with drugs, the
strength of studying proteomics in patient-derived tumor models is the
ability to test drug treatment in the mice,” Ding said. “With advances
in cancer proteomics that increase the speed of measurement, we are
moving toward a future that includes genomic and proteomic analyses of
patient tumors.”
Co-author Matthew J. Ellis, MD, PhD, of Baylor, agreed. “The mouse
work is promising enough to adapt these technologies for real time
analysis of patient materials so that clinical trials can be designed to
test this new diagnostic and drug selection approach,” he said.
Other key contributors to this project are Kuan-lin Huang, a PhD
student in genomics and bioinformatics at Washington University;
Shunqiang Li, PhD, an assistant professor of medicine at Washington
University; Philipp Mertins, PhD, of The Broad Institute; and Sherri
Davies, a senior scientist at Washington University.