Author : Dr Nima Afshar Assistant Clinical Professor of Medicine University of California San Francisco
2008-10-18
2008-10-18
KEY POINTS
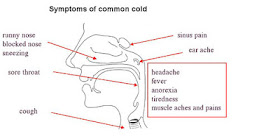
- The common cold is the most common illness in humans. The syndrome of runny nose, stuffed nose, sneezing, sore throat, and nagging cough is known to us all.
- A cold is a type of upper respiratory tract infection. Specifically, it is an infection of the nose and throat by a virus, the classic one being rhinovirus. There are over one hundred species of rhinovirus, which is a major reason why we keep catching colds.
- Young children, whose immune systems are naïve to the viruses, are the most vulnerable to colds, though adults still catch an average of 2-3 per year.[1-3] Colds are contagious, especially during the first few days of illness, and are spread through the air or by contaminated surfaces. A typical bout lasts one week.
- The common cold is a self-limited, usually mild illness. No treatment has been adequately proven to shorten its duration. Nevertheless, many traditional and alternative treatments exist to alleviate symptoms.
- Hand cleaning and avoiding prolonged close contact with someone that has a cold may prevent spread.
PERSPECTIVE
Epidemiology: Where, when, and how often colds occur
The common cold occurs throughout the world. In temperate climates colds tend to occur in cold weather months, while in tropical climates they occur during rainy months. In the U.S. rates of infection rise sharply in the late summer, when children return to school, and continue to be high until early spring.[4] Peak seasons may differ slightly in other regions of the world; a study of college students in Finland revealed the highest rates of infection in late winter and early spring.[5]The reasons for seasonal variation are not fully understood. It may be due in part to greater time spent indoors during cold seasons (or rainy seasons in the tropics), thereby increasing the chance of transmission of virus. It is also possible that cold weather itself contributes, perhaps by weakening the immune response to viruses, particularly in the nose.[6]
Americans suffer about 600 million colds every year*. Children are most vulnerable; before the age of 5 they have an average of 5-6 episodes per year (more if they are in day care). The incidence gradually decreases thereafter until adulthood, where it reaches about 2 episodes per year in men and 3 episodes per year in women; the difference is probably due to women having greater exposure to young children (data is from the 1960s and 70s). The elderly have only 1 cold annually (Figure 1).[3, 7]
Cost
The common cold is the #1 reason for visits to physicians and leads to almost 200 million missed school days and 200 million missed work days per year in the U.S. The total economic burden (considering both direct and indirect costs) is approximately $40 billion. This makes the common cold the 7th costliest disease in the U.S., which places it alongside serious conditions such as stroke.[1]Cold viruses are the major cause of flare-ups of asthma and COPD (chronic obstructive pulmonary disease, a medical term that encompasses emphysema and chronic bronchitis).[8] Such exacerbations are common and potentially serious, are a leading reason for hospitalization, and can even be fatal. These costs are not included in the above economic estimates.
Unnecessary antibiotic use is an often-unmeasured cost. One-sixth of adults and 1/3 of children with a cold seek medical care for their illness, and of these about 50% and 40%, respectively, receive antibiotics.[1] Such widespread antibiotic overuse leads to the development of resistant strains of dangerous bacteria, such as pneumococcus, the leading cause of pneumonia and meningitis. Those who recently used an antibiotic are at particular risk for carrying and becoming infected with such resistant organisms.[9]
* A study of 100 Cleveland families from the 1950s suggested about twice this number,[10] but more recent data[1, 3] probably better reflect the incidence in the less crowded U.S. households of today.
THE VIRUSES
Rhinovirus
Several groups of viruses cause colds (Table 1). The rhinoviruses are the dominant cold virus group, responsible for about half of all colds in adults and probably a similar proportion in children. In temperate climates their peak activity is in the fall, with a smaller peak in the spring. They are well-adapted to their role, as they grow best at 33°C, the typical temperature of the nasal passages. Their failure to grow well at typical internal body temperatures (~37°C) probably explains why they rarely invade the lungs or other internal organs and thus do not alone cause serious disease.The rhinovirus genus contains 100 species, which is one of the reasons that one never becomes fully immune to the cold. It is also the greatest impediment to development of a vaccine. Rhinoviruses are very small and possess a compact genome in the form of a single strand of RNA. Surrounding the RNA is a capsid (the shell of a virus) made up of multiple copies of 4 different proteins, which come together to form an icosahedron (a solid figure with 20 sides; there is no outer envelope. One section of the capsid forms a three-dimensional “canyon” that allows the virus to bind to the host cell membrane, initiating infection.[11] Table 1 -- Viruses that cause the Common Cold
Virus Group
|
% of Colds in Adults
|
| Rhinoviruses (100 types) |
~50
|
| Coronavirus (≥3 types) |
~10
|
| Influenza virus (3 types) |
5-10
|
| Parainfluenza virus (4 types) |
~4
|
| Respiratory syncytial virus – RSV (2 types) |
2-5
|
| Adenovirus (47 types) |
~1
|
| Other or unknown virus/organism |
~30
|
- Adapted from Gwaltney4 and Makela5
- Total percentage is >100% because co-infection with multiple viruses can occur
- Bacteria, not included in the table, cause ~4% of colds
The Rest
Coronavirus
- Coronaviruses are a genus of enveloped, single-stranded RNA viruses that are probably the second most common cause of the cold, though the exact percentage of colds due to coronaviruses is not known because they are difficult to isolate in the laboratory. Outbreaks occur mostly in winter and spring.
Influenza virus
- Influenza viruses typically cause the flu, a distinct syndrome that is more severe than the cold. But the two can overlap, which is why investigations into the etiology (cause) of the common cold usually find that influenza is the culprit in some cases. In older studies in which the technology available for detecting viruses was limited (causative agent identified in only 20-25% of cases), influenza represented 30% of pathogens,[3] but a more recent study employing sophisticated diagnostic techniques (thus identifying a causative agent in 70% of cases) found that influenza was associated with only 6% of colds.[5]
RSV
- Respiratory syncytial virus (RSV) is an important cause of colds in infants in winter. It can lead to an infection of the lower airways called bronchiolitis, which is a major cause of hospitalization in children less than 1 year old. RSV has been recently recognized as a culprit in severe respiratory infections in the elderly as well, with similar rates of hospitalization and even death as influenza.[12] Unlike influenza, however, RSV infection in most people produces a mild cold that is indistinguishable from that of a rhinovirus or coronavirus.
Other viruses
- In infants and young children, a cold due to parainfluenza virus can lead to croup, an infection of the vocal cords and trachea. This is a common and usually mild condition, but occasionally it causes enough swelling to impair breathing and require medical attention. Adenovirus, like influenza, can occasionally cause severe bouts of the cold.
Non-viruses
- Bacteria cause a very small percentage of colds in adults[5] and a somewhat higher percentage in children.[13] Regardless, colds due to bacteria are not more severe and nearly always resolve without antibiotics.[13, 14]
CATCHING THE COLD
Vulnerability
Infants and young children are most vulnerable to colds. Their immune systems are naïve to the multitude of strains of cold viruses (breastfed infants are partially immune because they acquire protective antibodies from the mother’s breast milk), they are often in close contact with other children, and they generally are not too concerned about personal hygiene. The latter two factors converge in toddlers in day care to produce so many colds (up to 10 per year) that at times they have yet to recover from one by the time they catch another. The good news is that children who attend day care are less vulnerable to colds later, in their preadolescent school years, compared to children who did not attend day care.[15] On the other hand, children who have unusually frequent colds as infants continue to catch them at a high rate into adolescence; they appear to have low levels of interferon, a natural anti-virus immune factor.[16] A variety of social environmental factors have been associated with a higher risk of colds:- Smoking: some studies show only that colds are more severe, while others show an increased number of colds[17, 18]
- Lack of alcohol: moderate alcohol consumption may decrease the risk of colds (in one study the association only held for red wine)[18, 19]
- Crowded home or work environments, including sharing bedrooms or office space[20]
- Stress: family, work[21]
- Social isolation: despite less contact with other potentially ill people[22]
- Fatigue and poor sleep[23]
- Night shift work[23]
- Poverty: perhaps due to multiple factors above[10]
Transmission
The contagiousness of colds is proportional to the concentration of virus in nasal secretions and the volume of those secretions. It is unlikely that colds are communicable before the onset of symptoms as secretions are absent or minimal. Rhinovirus is shed from the nasal lining as soon as symptoms begin. This shedding, along with the volume of nasal secretions, peaks on days 2-4. Both shedding and secretions then decrease quickly, though some virus may be shed for a couple weeks afterwards.[4] Thus colds are usually most contagious on days 2-4 of the illness.Rhinoviruses, the main group of cold viruses, are likely spread by 2 routes (other cold viruses use one or both of these):
1) Contact: Persons infected with rhinovirus have been shown to harbor the virus on their hands in 40% of cases. Even nearby objects can be contaminated with the virus, which can live on surfaces for hours to days. When a susceptible person gets the virus on their fingers, they then become infected by touching their nose or eyes. In an experiment, mothers who dipped their fingers in iodine periodically acquired fewer colds than mothers who dipped into a placebo solution. This suggested that direct (touching secretions) or indirect (touching contaminated surfaces) contact with the infected persons, in this case children at home, was a mode of transmission.[24] Interestingly, it appears that oral contact rarely transmits rhinovirus, so sharing drinks and even kissing are probably not risky in most colds.[24]
2) Airborne: The virus can also be spread by invisible droplets in the air – often released by sneezing and coughing. In a creative experiment, infected and well volunteers played poker in a room together for 12 hours. Half of the well volunteers either had their arms braced or their face shielded so that they could not touch their face. This half had almost the same infection rate as the unrestrained half (both close to 60%), strongly suggesting that something other than contact (by default, air exposure) was transmitting the virus.[24] The more time one spends with someone who has a cold (especially in close quarters), the higher the risk of airborne acquisition of the virus, even in the absence of physical contact.
Invasion
Rhinovirus begins its attack at the lining of the junction of the nose and throat. The canyon-like groove in the viral shell allows the virus to attach to a receptor called ICAM-1 on the surface of cells lining the back of the nose. The virus enters the host cell and begins its trickery. It hijacks the cell’s own machinery, using it to produce virus proteins that then shut down the cell’s own vital activities. Meanwhile, it continues to use the host cell’s machinery to make new copies of itself. The cell soon dies, releasing many virus particles that can continue the cycle in other cells. This process, from attack to new virus particles, takes less than 24 hours.[11]SYMPTOMS
Once the nasal cavity has been exposed to a cold virus, it takes as little as 8 hours to develop symptoms, though with some viruses this incubation period can be as long as 3 days. Initially, one often develops a vague sense of malaise (a feeling of illness), a scratchy throat, and/or the beginnings of a runny nose.[4] Within a day the full syndrome has usually taken hold (Figure 1), with the most common symptoms being:[13, 25]- Runny nose
- Congested nose
- Sneezing
- Sore throat
- Cough
Figure 1: Symptoms in 465 adults with colds. Data from Gwaltney et al. Rhinovirus infections in an industrial population. JAMA. 1967;202(6):494-500
Less common symptoms include headache, hoarseness, and muscle aches. Adults normally do not have a fever, and if they do it is low-grade (<38°C or 100.5°F). The duration of illness is typically 1 week, though in ¼ of cases symptoms remain for over 2 weeks.
Cough is often the major persistent problem, especially for women, smokers, and those with rhinovirus.[25] Why do some people still cough well after the virus has been cleared from the body? There are probably two reasons:
1) Airway inflammation: For some reason our body’s chemical mediators of inflammation can linger in the airway, which cause the sensory receptors of the cough reflex in the trachea and upper bronchi to lower their threshold for activation. This heightened airway sensitivity was demonstrated in volunteers with colds, in whom inhaling capsaicin (the chemical that gives peppers their spice) caused more coughing than it did in uninfected persons. That anti-inflammatory medications improve cough also supports this hypothesis.[26]
2) Post-nasal drip: Nasal secretions follow gravity, so they often run down the throat, where they can tickle the airway and induce coughing. This problem is more severe at night, when we are lying down, thus promoting drainage into the throat. Antihistamines that reduce runny nose may decrease coughing.[26]
Children have more symptoms than adults, and their illness lasts quite a bit longer (Figure 2). At 10 days of illness almost 75% of children still have some symptoms, versus only 20% of adults.[13]
 Figure
2: Symptoms in 81 children aged 5-12 with colds. Data from Pappas et
al. Symptom profile of common colds in school-aged children. The Pediatric Infectious Disease Journal. 2008;27(1):8-11.
Figure
2: Symptoms in 81 children aged 5-12 with colds. Data from Pappas et
al. Symptom profile of common colds in school-aged children. The Pediatric Infectious Disease Journal. 2008;27(1):8-11.
COMPLICATIONS
Although
the common cold is a benign illness in the vast majority of cases,
complications occur occasionally. By far the most important of these is
exacerbation of chronic lung disease. Persons with asthma or chronic
obstructive pulmonary disease (COPD) - which is nearly always caused by
smoking and includes emphysema and chronic bronchitis - often experience
flares of their underlying lung disease when infected with a cold
virus. Lung function worsens as airways narrow, producing symptoms such
as shortness of breath and wheezing that require medical attention.
When severe, these exacerbations require hospitalization – sometimes in
the intensive care unit for ventilator support – and can lead to death.
The bulk of costs, morbidity, and mortality from these chronic lung
diseases are attributable to flares, and about half of all flares and
most consequent hospitalizations are associated with cold viruses.[8]
This is important, as COPD alone is the 4th leading cause of death in
the U.S. A cold can also lead to bacterial infection of the sinuses or middle ear. During a cold excessive mucous may block passageways and back up into the sinuses and middle ear, creating a favorable environment for the growth of bacteria. Bacterial sinusitis causes fever, thick dark yellow or greenish nasal discharge, and facial pain. Bacterial middle ear infection, which occurs predominantly in infants and toddlers, causes fever and ear pain. Both conditions usually respond well to antibiotics.
IS THIS JUST A COLD?
Cold symptoms are so typical that one usually makes the correct self-diagnosis; medical tests are rarely needed. There are a few conditions, however, that can mimic a cold.Influenza/Flu
As mentioned previously, the common cold and the flu – a more severe syndrome caused by an influenza virus – overlap considerably, sometimes making the distinction difficult. The flu is also an upper respiratory tract infection, but it often also invades the lower respiratory tract and induces an intense immune response. The following are more common or more severe in flu than in a cold:- Fever: >38°C or 100.5°F
- Cough
- Headache
- Muscle aches
- Generalized weakness, fatigue, and loss of appetite
Fever and cough are especially predictive: the presence of both in a person with symptoms of an upper respiratory infection makes it 80% likely that the diagnosis is flu.[27] Time of year can be helpful as well. While colds are prevalent from fall through spring and even occur in summer, the flu is almost exclusively a winter disease, rarely occurring outside of the November-April timeframe. A doctor can confirm influenza infection by collecting nasal secretions and sending it to the lab for a rapid virus test. The diagnosis can be important because there are specific anti-viral treatments for the flu that if started early can shorten the course of the illness.
Allergies
Allergies such as hay fever (“allergic rhinitis” is the medical term) are caused by the immune system overreacting to harmless substances such as pollen or mold. The symptoms, particularly runny nose, nasal congestion, and sneezing, can be similar to a cold. The easiest way to distinguish allergies from cold is by the presence of itching. Itchiness of the eyes and palate (roof of the mouth) should not occur with a cold. Allergies are also much less likely to cause cough, sore throat, or systemic symptoms such as malaise and muscle aches.Strep throat
Both
a cold and strep throat, which is an infection of the throat by the
bacterial species called Group A Streptococcus, can cause a sore throat.
Strep throat, however, is associated with more severe throat pain that
makes it difficult to swallow. The throat is red and the tonsils have
yellowish spots. Lymph nodes in the front of the neck are usually
enlarged and tender. Fever and headache are common, while nasal
symptoms and cough are typically absent. Children may have abdominal
pain and occasionally even vomiting. Strep is most prevalent in 5-15
year olds, and is very uncommon before the age of 3. If needed, a
throat swab can confirm the diagnosis. Antibiotics prevent rare but
dangerous complications. Sometimes a viral infection called infectious
mononucleosis (“mono”) can behave just like strep throat; it is
diagnosed by a blood test. TREATMENT
The
common cold is a self-limited illness; that is, our immune systems cure
it nearly every time. Nevertheless, it is a burden that causes some
degree of suffering. Fortunately, treatments do exist that alleviate
the symptoms of the cold. Some are well-proven, some may work for a
subset of people, and some probably rarely work for anybody.
Below is a list of proposed or currently used treatments for the cold, our conclusions about their effectiveness, and in smaller print the details about how they work as well as a summary of the medical evidence for or against each treatment. In this section, we frequently refer to “randomized controlled trials.” These are studies in which patients are randomly assigned to receive either the treatment or a placebo – and are unaware of which they are taking. The effectiveness of the treatment is determined by comparing its impact on symptoms or other parameters to that of the placebo. Because there is often a substantial placebo effect (people feel better despite any biological explanation for improvement) in cold treatments, the randomized controlled study design is especially important to determine whether or not a treatment really works. It should also be noted that many treatments, including herbs and other alternative agents, have not been thoroughly tested. This does not mean that they do not work – it simply means that from a scientific perspective, we don’t know whether or not they work.
*Hand cleaning: The hands are the vehicle for transmitting the cold virus in both the infected and uninfected person. Washing hands with water and soap probably helps to lower virus counts on the hand. Alcohol-based gels appear to be far superior to hand washing for removing viruses (as well as bacteria) from the hand.[42]
Below is a list of proposed or currently used treatments for the cold, our conclusions about their effectiveness, and in smaller print the details about how they work as well as a summary of the medical evidence for or against each treatment. In this section, we frequently refer to “randomized controlled trials.” These are studies in which patients are randomly assigned to receive either the treatment or a placebo – and are unaware of which they are taking. The effectiveness of the treatment is determined by comparing its impact on symptoms or other parameters to that of the placebo. Because there is often a substantial placebo effect (people feel better despite any biological explanation for improvement) in cold treatments, the randomized controlled study design is especially important to determine whether or not a treatment really works. It should also be noted that many treatments, including herbs and other alternative agents, have not been thoroughly tested. This does not mean that they do not work – it simply means that from a scientific perspective, we don’t know whether or not they work.
Pain and Fever Medications
· Acetaminophen/Paracetamol (Tylenol): Effective. Should be the first-line pain reliever and fever reducer for most people.
o How
acetaminophen, better known internationally as paracetamol, relieves
pain is still being studied. It may work in part by blocking an enzyme
called COX that mediates inflammation (though somehow this does not lead
to a significant anti-inflammatory effect), but new evidence shows that
perhaps it mostly works by indirectly stimulating cannabanoid
receptors, the same ones that are stimulated by THC, the active
ingredient in marijuana.
o Few
randomized controlled trials have tested acetaminophen in patients with
colds, but all of them have shown a substantial benefit over placebo
for reduction of pain – sore throat, muscle aches, headache – as well as
reduction of fever, in both adults and children.[28] Besides these
small studies, this medication has a long track record of efficacy in
the experience of physicians and the public. Acetaminophen is very safe
when taken at recommended doses. The total dose of acetaminophen
should never exceed 4 grams per 24 hours – note that acetaminophen is a
part of many combination prescription narcotic medications such as
Vicodin and Percocet, so its dose in these preparations must be added to
the dose from any other form (i.e., Tylenol) to come up with the total
dose taken. Exceeding the recommended dose can lead to life-threatening
liver damage.
· NSAIDs – Ibuprofen (Motrin, Advil), Naproxen (Alleve): Effective.
o NSAID
stands for “non-steroidal anti-inflammatory drug.” These drugs work by
blocking COX, an enzyme that promotes inflammation.
o
Like acetaminophen, NSAIDs have been sparsely tested in patients with
colds. The studies that do exist, mostly using ibuprofen, have shown a
similar benefit for pain and fever compared to acetaminophen, in both
adults and children. NSAIDs are generally safe, though there are a few
potential serious side effects: gastrointestinal bleeding, kidney
dysfunction, and allergic reactions. The first two problems are rarely
seen with short-term use, unless one is susceptible (e.g., a history of
stomach bleeding or pre-existing kidney disease). Allergic reactions
can occur with any medication, but are more common with NSAIDs than
acetaminophen. Of note, aspirin is another NSAID, but it is not
recommended for pain or fever as it has more frequent and dangerous side
effects compared to other NSAIDs without any additional benefit.[28]
Decongestants
· Topical – Oxymetazoline (Afrin) and others: Effective for nasal congestion.
o Topical
decongestants usually are in the form of sprays that deliver
vasoconstrictors to the nasal lining; these shrink the enlarged blood
vessels that cause congestion.
o
Two randomized controlled trials with a total of ~900 patients showed
that these medications provide substantial relief of nasal
congestion.[29, 30] They should not be used for more than 3 days, as
doing so may cause a rebound effect leading to recurrent congestion.
· Oral – Phenylephrine (Sudafed PE), Pseudoephedrine (Sudafed), and others: Minimally effective for nasal congestion.
o
These medications are also vasoconstrictors that get to the nasal
lining via the bloodstream (after being absorbed across the intestines).
o A
review of 6 randomized controlled trials with a total of ~650 patients
concluded that oral decongestants (pseudoephedrine mainly studied)
provide minimal benefit – only about a 5% reduction in congestion.[31]
Because they get absorbed into the bloodstream and they act by
constricting blood vessels, they can sometimes cause a modest elevation
of high blood pressure. This is not a problem in people whose blood
pressure is well-controlled, but it can be dangerous for those with
uncontrolled hypertension or certain medical conditions. Because
pseudoephedrine can be used to synthesize methamphetamine, an
increasingly common drug of abuse, sales of this drug in the U.S. are
now limited and regulated. Thus, phenylephrine is becoming a more
common ingredient in over-the-counter preparations, though it has not
been tested adequately and may not be effective.
Antihistamines
· First-generation – Diphenhydramine (Benadryl) and others: Modestly effective for runny nose.
o These
drugs block histamine, a compound in the body that causes allergies.
They also block acetylcholine, a neurotransmitter that leads to
secretions in the nose and airway.
o A
review of 27 randomized controlled trials including thousands of
patients found that this class of medication has minimal benefit for
runny nose - certainly <15% improvement. The side effect of sedation
limits use for some during the day, though in the above this effect was
surprisingly small (only 3% more than placebo).[32] The elderly and
those with even mild dementia should avoid these medications, as they
can cause severe sleepiness and/or confusion in such persons.
· Non-sedating – Loratidine (Claritin), Fexofenadine (Allegra): Ineffective.
o
These second-generation antihistamines do not get into the brain, so
they spare most of the side effects of the first-generation class.
o They
were developed for allergies (and are effective in this setting),
though they are sometimes used for colds as well. A review of 8
randomized controlled trials showed no benefit for these medications in
patients with colds.[32]
Cough medications
· Guiafenisin: Possibly effective.
o
This drug is an expectorant. It works by loosening secretions so that
they are better expectorated (coughed out), leaving fewer secretions
behind, thus reducing an airway irritant that causes cough.
o Two
randomized controlled trials have been done. The larger one, with 239
patients, found a 75% reduction of cough in the treatment group vs. 31%
reduction in the placebo group. The smaller one, with 65 patients,
found no reduction in cough but a 40% reduction in phlegm thickness.[33]
· Dextromethorphan: Questionably effective.
o Dextromethorphan
is thought to suppress cough by multiple mechanisms of action,
including activation of opioid receptors in the brain.
o
One meta-analysis of 6 pharmaceutical company-sponsored randomized
controlled trials totaling 710 patients showed an average of a 15%
reduction in various cough parameters with dextromethorphan (an earlier
meta-analysis in the literature likely included the same original
studies). Two smaller trials (48 and 108 patients) showed no reduction
in cough in patients with colds.[34]
· Codeine: Probably not effective.
o Codeine is thought to suppress by activating opioid receptors in the brain.
o Two
randomized controlled trials with 80 patients each failed to show any
reduction of coughing with codeine in patients with colds.[33]
Vitamins/Minerals and Herbs
· Vitamin C: Ineffective.
o
Vitamin C in the treatment of colds has been extensively studied:
several randomized controlled trials totaling ~3000 patients assessed
its effect on cold duration and/or severity. In aggregate the data
show no benefit for either parameter.
· Zinc: Lozenges probably not effective. Topical forms should be avoided due to reports of permanent loss of smell.
o
Twelve randomized controlled trials totaling ~1600 patients have
assessed zinc lozenges for the treatment of colds, with duration and
severity of symptoms being the major parameters measured. Six studies
showed some benefit, 4 showed no benefit, and 2 showed harm. The 4
studies showing no benefit were large – about 1000 total patients were
included in these studies alone.[35]
o
Four randomized controlled trials totaling ~540 patients have assessed
topical zinc applied directly into the nasal passages. One used a
low-dose nasal spray and found marginal to no benefit. One study used a
high-dose gel in experimentally induced colds and found no benefit.
Two studies used a high-dose gel in natural colds and found significant
benefit.[35] Regardless, there have been case reports of severe or
total loss of smell after use of intranasal zinc,[36] so this form of
the mineral should be avoided.
· Echinacea: Flower and stem portion of the plant may reduce duration of symptoms.
o
Echinacea has been used as a medicinal herb by Native Americans for
centuries and is now among the most popular herbs in the U.S. Numerous
studies, with a total of ~1600 patients, have tested this herb as a
treatment for colds. The results have been quite mixed. One review of
all these studies concluded that there was not convincing evidence of
benefit (due to wide variation in study results and the fact that
several studies that were never published showed no benefit),[37] while
another review concluded that Echinacea reduced duration of colds by 1.5
days.[38] The former review mentioned that Echinacea preparations vary
greatly in content; the ones composed of the aerial parts of the plant
(flower, stem) appeared to be more effective.
· Chinese herbs: Not well studied. No recommendations.
o There
are a multitude of Chinese herbs used for the common cold. Studies of
them have generally been of poor quality and have had mixed results.[39]
From a scientific perspective, we do not yet know whether or not any
of these herbs are effective.
Miscellaneous
· Antibiotics: No role in the treatment of a cold.
o
Two major literature reviews have been done. Seven studies were
found that assessed the effect of antibiotics for the common cold.
Pooling all the results, there was no benefit for most outcomes: no
reduction in duration of the cold or severity of most symptoms; there
was mild benefit for runny nose. Only two studies used an antibiotic
that is commonly prescribed today in the U.S. (amoxicillin); they showed
no benefit for most outcomes, though there was a mild reduction in
thick nasal discharge with antibiotics. Antibiotics caused diarrhea in
10% of patients.[14, 40]
· Heated, humidified air: Unlikely to reduce severity of symptoms.
o
Hot tea and soup have been used for centuries. Scientists theorized
and found preliminary evidence supporting the idea that high nasal
temperatures could destroy rhinovirus. A machine called Rhinotherm was
developed to deliver hot, humidified air directly to the nasal passages.
This and similar machines have been tested in 6 studies. Three (2 in
U.K., 1 in Israel) found major benefit in symptoms and objective
measures of nasal patency (openness), while all 3 done in the U.S. found
no benefit in either of these endpoints (one even found decreased nasal
patency). So this specific treatment cannot be recommended in the U.S.
A large study is needed to resolve the discrepancies in the results of
the above studies.[41]
PREVENTION
Prevention of the spread of cold viruses from infected to uninfected persons requires combating the known mechanisms of viral transmission by cleaning one’s hands frequently and limiting airborne exposure.*Hand cleaning: The hands are the vehicle for transmitting the cold virus in both the infected and uninfected person. Washing hands with water and soap probably helps to lower virus counts on the hand. Alcohol-based gels appear to be far superior to hand washing for removing viruses (as well as bacteria) from the hand.[42]
*Limiting
airborne exposure: Duration of close proximity between those with and
those without colds, even in the absence of physical contact, increases
the risk of transmitting the virus. So limiting the amount of time
spent in small rooms together may reduce this risk. Also, those with
colds can practice simple hygiene measures such as sneezing into
disposable tissues or coughing/sneezing onto a sleeve rather than into
the hands.
We never stop getting colds. There a total of almost 200 strains of all cold viruses. When we are infected with one of them we develop immunity to it, with some cross-immunity against other similar strains. This immunity wanes over time, so we can be infected by the same strain in the future, though symptoms are usually mild in such cases. Attacks are most severe when we are exposed to an unusual strain. The sheer number of strains and our imperfect immunity limit the potential for a vaccine.
In the end, a vaccine was probably never realistic. We appear to be destined to live with the ritual nuisance of the common cold for quite some time.
“I enjoy convalescence. It is the part that makes the illness worth while.”
-George Bernard Shaw
We never stop getting colds. There a total of almost 200 strains of all cold viruses. When we are infected with one of them we develop immunity to it, with some cross-immunity against other similar strains. This immunity wanes over time, so we can be infected by the same strain in the future, though symptoms are usually mild in such cases. Attacks are most severe when we are exposed to an unusual strain. The sheer number of strains and our imperfect immunity limit the potential for a vaccine.
In the end, a vaccine was probably never realistic. We appear to be destined to live with the ritual nuisance of the common cold for quite some time.
“I enjoy convalescence. It is the part that makes the illness worth while.”
-George Bernard Shaw
REFERENCES
1. Fendrick
AM, Monto AS, Nightengale B, Sarnes M. The economic burden of
non-influenza-related viral respiratory tract infection in the United
States. Arch Intern Med 2003;163(4):487-94.
2. Gwaltney
JM, Jr., Hendley JO, Simon G, Jordan WS, Jr. Rhinovirus infections in
an industrial population. I. The occurrence of illness. N Engl J Med
1966;275(23):1261-8.
3. Monto AS, Sullivan
KM. Acute respiratory illness in the community. Frequency of illness and
the agents involved. Epidemiol Infect 1993;110(1):145-60.
4. Gwaltney
JM, Jr. Common Cold. In: Mandell, Douglas, and Bennett's Principles and
Practice of Infectious Diseases, 6th ed.: Elsevier; 2005.
5. Makela
MJ, Puhakka T, Ruuskanen O, et al. Viruses and bacteria in the etiology
of the common cold. J Clin Microbiol 1998;36(2):539-42.
6. Eccles
R. An explanation for the seasonality of acute upper respiratory tract
viral infections. Acta Otolaryngol (Stockh) 2002;122(2):183-91.
7. Monto AS, Ullman BM. Acute respiratory illness in an American community. The Tecumseh study. Jama 1974;227(2):164-9.
8. Mallia P, Johnston SL. How viral infections cause exacerbation of airway diseases. Chest 2006;130(4):1203-10.
9. Nuermberger
EL, Bishai WR. Antibiotic resistance in Streptococcus pneumoniae: what
does the future hold? Clin Infect Dis 2004;38 Suppl 4:S363-71.
10. Monto AS. Epidemiology of viral respiratory infections. Am J Med 2002;112 Suppl 6A:4S-12S.
11. Dreschers
S, Dumitru CA, Adams C, Gulbins E. The cold case: are rhinoviruses
perfectly adapted pathogens? Cell Mol Life Sci 2007;64(2):181-91.
12. Falsey
AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial
virus infection in elderly and high-risk adults. N Engl J Med
2005;352(17):1749-59.
13. Pappas DE, Hendley
JO, Hayden FG, Winther B. Symptom Profile of Common Colds in School-Aged
Children. The Pediatric Infectious Disease Journal 2008;27(1):8-11.
14. Arroll
B, Kenealy T. Are antibiotics effective for acute purulent rhinitis?
Systematic review and meta-analysis of placebo controlled randomised
trials.[see comment]. Bmj 2006;333(7562):279.
15. Ball
TM, Holberg CJ, Aldous MB, Martinez FD, Wright AL. Influence of
attendance at day care on the common cold from birth through 13 years of
age.[see comment]. Arch Pediatr Adolesc Med 2002;156(2):121-6.
16. Ball TM, Holberg CJ, Martinez FD, Wright AL. Is there a common cold constitution? Ambul Pediatr 2002;2(4):261-7.
17. Bensenor IM, Cook NR, Lee IM, et al. Active and passive smoking and risk of colds in women. Ann Epidemiol 2001;11(4):225-31.
18. Cohen
S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP. Smoking, alcohol
consumption, and susceptibility to the common cold. Am J Public Health
1993;83(9):1277-83.
19. Takkouche B,
Regueira-Mendez C, Garcia-Closas R, Figueiras A, Gestal-Otero JJ, Hernan
MA. Intake of wine, beer, and spirits and the risk of clinical common
cold. Am J Epidemiol 2002;155(9):853-8.
20. Jaakkola JJ, Heinonen OP. Shared office space and the risk of the common cold. Eur J Epidemiol 1995;11(2):213-6.
21. Cohen S, Tyrrell DA, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991;325(9):606-12.
22. Cohen
S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM, Jr. Social ties and
susceptibility to the common cold. Jama 1997;277(24):1940-4.
23. Mohren
DCL, Jansen NWH, Kant IJ, Galama J, van den Brandt PA, Swaen GMH.
Prevalence of common infections among employees in different work
schedules. J Occup Environ Med 2002;44(11):1003-11.
24. Goldmann DA. Transmission of viral respiratory infections in the home. Pediatr Infect Dis J 2000;19(10 Suppl):S97-102.
25. Gwaltney
JM, Jr., Hendley JO, Simon G, Jordan WS, Jr. Rhinovirus infections in
an industrial population. II. Characteristics of illness and antibody
response. Jama 1967;202(6):494-500.
26. Pratter MR. Cough and the common cold: ACCP evidence-based clinical practice guidelines. Chest 2006;129(1 Suppl):72S-4S.
27. Eccles R. Mechanisms of symptoms of the common cold and influenza. Br J Hosp Med (Lond) 2007;68(2):71-5.
28. Eccles
R. Efficacy and safety of over-the-counter analgesics in the treatment
of common cold and flu. J Clin Pharm Ther 2006;31(4):309-19.
29. Eccles
R, Pedersen A, Regberg D, Tulento H, Borum P, Stjarne P. Efficacy and
safety of topical combinations of ipratropium and xylometazoline for the
treatment of symptoms of runny nose and nasal congestion associated
with acute upper respiratory tract infection. Am J Rhinol
2007;21(1):40-5.
30. Akerlund A, Klint T, Olen
L, Rundcrantz H. Nasal decongestant effect of oxymetazoline in the
common cold: an objective dose-response study in 106 patients. J
Laryngol Otol 1989;103(8):743-6.
31. Taverner D, Latte J. Nasal decongestants for the common cold. Cochrane Database Syst Rev 2007(1):CD001953.
32. Sutter
AIM, Lemiengre M, Campbell H, Mackinnon HF. Antihistamines for the
common cold. Cochrane Database Syst Rev 2003(3):CD001267.
33. Smith
SM, Schroeder K, Fahey T. Over-the-counter medications for acute cough
in children and adults in ambulatory settings. Cochrane Database Syst
Rev 2008(Issue 1. Art. No.: CD001831. DOI:
10.1002/14651858.CD001831.pub3.).
34. Bolser
DC. Cough suppressant and pharmacologic protussive therapy: ACCP
evidence-based clinical practice guidelines. Chest 2006;129(1
Suppl):238S-49S.
35. Hulisz D. Efficacy of zinc against common cold viruses: an overview. J Am Pharm Assoc (2003) 2004;44(5):594-603.
36. Jafek BW, Linschoten MR, Murrow BW. Anosmia after intranasal zinc gluconate use. Am J Rhinol 2004;18(3):137-41.
37. Linde
K, Barrett B, Wolkart K, Bauer R, Melchart D. Echinacea for preventing
and treating the common cold. Cochrane Database Syst Rev
2006(1):CD000530.
38. Shah SA, Sander S, White
CM, Rinaldi M, Coleman CI. Evaluation of echinacea for the prevention
and treatment of the common cold: a meta-analysis. Lancet Infect Dis
2007;7(7):473-80.
39. Wu T, Zhang J, Qiu Y, Xie L, Liu GJ. Chinese medicinal herbs for the common cold. Cochrane Database Syst Rev 2007(1):CD004782.
40. Arroll B, Kenealy T. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev 2005(3):CD000247.
41. Singh M. Heated, humidified air for the common cold. Cochrane Database Syst Rev 2006;3:CD001728.
42. Boyce
JM, Pittet D, Healthcare Infection Control Practices Advisory C, Force
HSAIHHT. Guideline for Hand Hygiene in Health-Care Settings.
Recommendations of the Healthcare Infection Control Practices Advisory
Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society
for Healthcare Epidemiology of America/Association for Professionals in
Infection Control/Infectious Diseases Society of America. MMWR Recomm
Rep;51(RR-16):1-45.