Author: Dr Richard P Kraig University of Chicago 2008-07-24
Migraine: Mechanisms and Management.
Migraine is the most common form of headache for which patients seek medical attention. Migraine also is an immense health care burden to those who suffer from this malady, as well as to society in general.
Migraine: Mechanisms and Management.
Migraine is the most common form of headache for which patients seek medical attention. Migraine also is an immense health care burden to those who suffer from this malady, as well as to society in general.
INTRODUCTION
Migraine is the most common form of headache for which patients seek medical attention [1]. Migraine also is an immense health care burden to those who suffer from this malady, as well as to society in general [2]. My focus here will be two-fold. First, I will explain how a migraine is thought to occur and how effective treatments are likely to work, since improved understanding can help control the headaches [3]. Second, I will emphasize that, while migraine is often driven to occur by altered genes, this fact does not mean a patient with migraine has been sentenced to a lifetime of head pain [4]. Instead, increasing evidence shows that the altered genes that cause migraine enhance only the likelihood a migraine will develop. Importantly, the tendency to develop disease (like migraine) can be reversed by environment, that is, how one lives. I will elaborate below, but it can be a tremendously empowering notion for patients when they understand they can improve their neurological health through physical, social and intellectual activity.WHAT IS MIGRAINE?
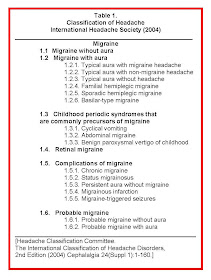
Accurate classification of headache types can improve patient care as well as research into the causes and treatment of headache. As a result, the International Headache Society completed an updated classification of headaches [5]. This compilation categorizes headaches as “primary” or “secondary.” Secondary headaches areMigraine is a periodic headache that can occur with various neurological, behavioral or gastrointestinal changes [TABLE 1].
Migraine is defined as a headache that [TABLE 2]:
(A) Has occurred at least five times;
(B) With each headache episode lasting 4-72 hours (either treated or untreated);
(C) With the pain having at least two of the following characteristics:
- Localized to one side of the head;
- Throbbing nature;
- Moderate to severe intensity;
- Worsened by routine physical activity, such as walking or climbing stairs.
(D) In addition, the patient must complain that:
- They are nauseated and/or vomit during the headache;
- They have increased sensitivity to light or sound.
(E) Finally, the headache cannot be attributed to another cause; it is not a “secondary” headache.
In addition to the above defining characteristics of head pain that must occur at least two times, migraine with aura [TABLE 2] must also:
(A) Show evidence of fully reversible neurological changes involving visual, sensory, or language symptoms;
(B) Have neurological symptoms consisting of:
- At
least two fully reversible visual, sensory, or language (i.e., loss of
language function (aphasia)) alterations that start before the headache
(or occur with the headache). “Homonymous positive features” refers to
visual changes that are defined as a change in vision that gets in the
way of normal vision. Typically this consists of flickering spots
(obscurations) that are seen in one half of the visual field as shown in
the video to the right [see Video 1 below]. Then, vision is reduced or
lost (a scotoma) behind the obscuration, as both move across the
patient’s visual field.
In the case of touch, a patient might feel pins and needles before feeling numb on one side of the body. For language, patients report an inability to express themselves correctly – that is, they become aphasic. - These neurological changes need to develop gradually over greater than five minutes or occur greater than two times in succession – with each change lasting five to 60 minutes.
(D) They then need to be followed (within five to 60 minutes) by a headache that is most commonly reported on a part of the head opposite to the side of body with the visual or body sensory change.
(E) Again, the headache and aura cannot be attributed to any other cause. Otherwise, it would be a secondary headache.
WHAT CAUSES MIGRAINE?
Three aspects of the above characteristics of migraine aura point to how the brain produces it. For our purposes here, we will focus on visual aura, though the concepts can be applied to all other types of migraine aura.First, patients experience a positive obscuration that moves slowly across one half of their field of vision. This is similar to the moon at night moving from the highest point in the sky to the horizon as dawn approaches. Second, as the obscuration moves, it is followed by a loss of vision – a blind spot in the visual field called a scotoma – which moves behind the obscuration. Third, movement is slow. The importance of that is linked to the 1941 observation of a scientist, named Lashley, who suffered from migraine.
In 1941 Lashley clocked the progression of his own visual aura. It took 22 minutes for Lashley’s aura to travel across his visual field, a distance of 67 millimeters in the occipital cortex. As a result, Lashley concluded that his visual aura traveled at three millimeters a minute in his brain. He published this observation in 1941 [6].
For the brain, this is an immensely slow time. For example, neural signals that arise from stubbing a toe travel all the way to the top of the brain (cerebral cortex) in less than a second. In contrast, the migraine visual aura’s speed of three millimeters per minute was the slowest process known at the time. In fact, only one brain process discovered in the last sixty years moves at this remarkably slow speed. It is called spreading depression.
Spreading depression was discovered by a Brazilian scientist studying at the Massachusetts General Hospital where he was recording brain electrical activity. This scientist, Leão, first reported his results in 1941 [7] and termed his discovery “spreading depression.” Since then, most researchers have concluded that the aura of migraine stems from spreading depression. Others, including me, have shown that spreading depression is also the most likely cause of migraine pain (see below) but first we’ll deal with the aura.
Leão defined spreading depression by three characteristics. First, it occurs with a transient loss of all brain electrical activity (depression). Second, this loss of activity occurs with a large potential shift to the negative outside of brain cells (which reflects their depression). Third and most importantly, these two changes move over the involved areas of the brain (spreading) at a rate of three millimeters a minute - thus, spreading depression (a spreading, transient loss of brain function). The cartoon shows a slice of brain that can be used to trigger spreading depression from a twisted wire electrical stimulating electrode shown to the lower right. To the left is a small needle electrode used to record the spreading depression shown as the moving line. Notice that:
(1) Normal brain electrical activity is seen as the short-lived vertical deflections in the line (1);
(2) Then as spreading depression is about to occur, neuronal activity briefly increases (2);
(3) Next, and probably due to this flurry of increased neuronal activity, a blast of synchronous neuronal discharges triggers the onset of spreading depression (3);
(4) Which is quickly followed by a large negative potential wave (4). The second video [video 3] shows this wave of depression traveling across a slice of brain just as it would over brain in patients experiencing migraine.
While a brief electrical pulse can be used
to excite the brain to trigger spreading depression in the brain slices,
it is fair to ask how this might occur in patients and so result in
migraine aura and headache.
The answer is that the brain of those who experience migraines (migraineurs) is more excitable than those who do not suffer from this type of headache. As a result, normal stimuli from sounds, smells or vision can be enough to over-excite brain and so cause it to trigger a spreading depression – and resultant migraine. For example, Aurora and colleagues flashed visual stimuli at patients with migraine and measured the electrical activity at the visual cortex [8]. Not only were the brains of these patients more responsive to the visual stimuli, the flashing stimuli could actually trigger a migraine aura and headache in susceptible patients.
The fact that the brain of migraineurs is more excitable than normal takes on added importance when one considers a fascinating chemical reaction that can be demonstrated in a Petri dish. The reaction is called a Belousov-Zhabotinsky reaction [9]. When special chemicals are mixed in a dish and made sufficiently excitable at a triggering point, a slowly propagating chemical oscillation is created – much like the flashing visual stimulus used by Aurora and colleagues that evoked the aura of migraine. As a result, recurrent waves begin to travel from the stimulus point, like waves from the sea coming ashore as shown in the video. Remarkably these waves travel at three millimeters a minute, just like spreading depression.
The reactants for the Belousov-Zhabotinsky reaction are evenly distributed and lie quietly throughout the Petri dish until activated at a stimulus point to trigger the diffusing reaction. In the brain such evenly distributed “chemicals” take the form of synapses to create a similar reaction – spreading depression.
In the brain, synapses are the areas where neurons communicate and there are two key types at play in migraine: The excitatory and inhibitory synapses. Excitatory synapses increase brain activity and inhibitory synapses reduce it. Spreading depression begins because of a loss of inhibition at the neuronal cell bodies. This is the key activity change behind spreading depression.
For those interested in more detail, synapses are the localized areas at which one neuron talks to another. Collectively, these excitatory and inhibitory synapses make up the electrical activity by which the brain works. It’s easy to see that brain can become over-excited by either an increase in excitation or a decrease in inhibition at these synapses. For example, a moving car might be likened to brain activity if driven while stepping on the gas with one foot, the other is stepping on the brake. The foot on the gas pedal represents excitatory synapses. The foot on the brake represents inhibitory synapses. If the gas pedal is pressed or a foot taken off the brake, the car would move faster. Suddenly traveling faster by taking a foot off the brake is how spreading depression begins.
Recent measurements of the electrical currents that travel through brain cells to create brain activity show that spreading depression begins because of a loss of inhibition at neuronal cell bodies [10]. As I mentioned above, electrical changes of spreading depression show four basic changes: (1) normal activity is briefly increased (2) a flurry of neuronal activity occurs, which likely corresponds to the positive visual obscuration of migraine aura. Next (3), the flurry of increased activity causes a group of brain cells to become active in unison, triggering spreading depression which becomes evident as (4) a loss of all brain activity. While I will explain this in further below for those interested in specific details but the important take home message is this: spreading depression begins with a loss of brain cell inhibition.
The four steps of spreading depression have corresponding changes in brain cell currents that flow across their cell membranes. The cartoon shows a typical neuron in brain (yellow) with excitatory (E) synapses in blue and inhibitory synapses in red (I).
(1) As neurons are activated under normal circumstances, current first flows into cells (blue arrows) and then out (red arrows) at the excitatory and inhibitory synapses.
(2) With the flurry of neuronal activity that occurs with the positive visual obscuration of migraine aura, these same currents increase in frequency.
(3) As a result, suddenly normal activity (NL) is transformed as by a reversal of current flow for a few seconds over a wide expanse of brain tissue that becomes the trigger zone of spreading depression (SDT).
(4) From this starting point, spreading depression emerges as a propagating reaction-diffusion wave (SDR/D) of electrical silence where all synapses go silent (gray) before all returns to normal in about two minutes.
The answer is that the brain of those who experience migraines (migraineurs) is more excitable than those who do not suffer from this type of headache. As a result, normal stimuli from sounds, smells or vision can be enough to over-excite brain and so cause it to trigger a spreading depression – and resultant migraine. For example, Aurora and colleagues flashed visual stimuli at patients with migraine and measured the electrical activity at the visual cortex [8]. Not only were the brains of these patients more responsive to the visual stimuli, the flashing stimuli could actually trigger a migraine aura and headache in susceptible patients.
The fact that the brain of migraineurs is more excitable than normal takes on added importance when one considers a fascinating chemical reaction that can be demonstrated in a Petri dish. The reaction is called a Belousov-Zhabotinsky reaction [9]. When special chemicals are mixed in a dish and made sufficiently excitable at a triggering point, a slowly propagating chemical oscillation is created – much like the flashing visual stimulus used by Aurora and colleagues that evoked the aura of migraine. As a result, recurrent waves begin to travel from the stimulus point, like waves from the sea coming ashore as shown in the video. Remarkably these waves travel at three millimeters a minute, just like spreading depression.
The reactants for the Belousov-Zhabotinsky reaction are evenly distributed and lie quietly throughout the Petri dish until activated at a stimulus point to trigger the diffusing reaction. In the brain such evenly distributed “chemicals” take the form of synapses to create a similar reaction – spreading depression.
In the brain, synapses are the areas where neurons communicate and there are two key types at play in migraine: The excitatory and inhibitory synapses. Excitatory synapses increase brain activity and inhibitory synapses reduce it. Spreading depression begins because of a loss of inhibition at the neuronal cell bodies. This is the key activity change behind spreading depression.
For those interested in more detail, synapses are the localized areas at which one neuron talks to another. Collectively, these excitatory and inhibitory synapses make up the electrical activity by which the brain works. It’s easy to see that brain can become over-excited by either an increase in excitation or a decrease in inhibition at these synapses. For example, a moving car might be likened to brain activity if driven while stepping on the gas with one foot, the other is stepping on the brake. The foot on the gas pedal represents excitatory synapses. The foot on the brake represents inhibitory synapses. If the gas pedal is pressed or a foot taken off the brake, the car would move faster. Suddenly traveling faster by taking a foot off the brake is how spreading depression begins.
Recent measurements of the electrical currents that travel through brain cells to create brain activity show that spreading depression begins because of a loss of inhibition at neuronal cell bodies [10]. As I mentioned above, electrical changes of spreading depression show four basic changes: (1) normal activity is briefly increased (2) a flurry of neuronal activity occurs, which likely corresponds to the positive visual obscuration of migraine aura. Next (3), the flurry of increased activity causes a group of brain cells to become active in unison, triggering spreading depression which becomes evident as (4) a loss of all brain activity. While I will explain this in further below for those interested in specific details but the important take home message is this: spreading depression begins with a loss of brain cell inhibition.
The four steps of spreading depression have corresponding changes in brain cell currents that flow across their cell membranes. The cartoon shows a typical neuron in brain (yellow) with excitatory (E) synapses in blue and inhibitory synapses in red (I).
(1) As neurons are activated under normal circumstances, current first flows into cells (blue arrows) and then out (red arrows) at the excitatory and inhibitory synapses.
(2) With the flurry of neuronal activity that occurs with the positive visual obscuration of migraine aura, these same currents increase in frequency.
(3) As a result, suddenly normal activity (NL) is transformed as by a reversal of current flow for a few seconds over a wide expanse of brain tissue that becomes the trigger zone of spreading depression (SDT).
(4) From this starting point, spreading depression emerges as a propagating reaction-diffusion wave (SDR/D) of electrical silence where all synapses go silent (gray) before all returns to normal in about two minutes.
Again, the important take-home message here is that spreading depression begins with a loss of brain cell inhibition.
Loss of inhibition can be seen with seizures and is a basis for use of anticonvulsants as a means to restore inhibition – and so stop seizures. Perhaps, a similar loss of inhibition in migraine is why anticonvulsants can stop migraine over time. Spreading depression-like events have been seen in patients during migraine [11, 12].
Loss of inhibition can be seen with seizures and is a basis for use of anticonvulsants as a means to restore inhibition – and so stop seizures. Perhaps, a similar loss of inhibition in migraine is why anticonvulsants can stop migraine over time. Spreading depression-like events have been seen in patients during migraine [11, 12].
Finally, how can spreading depression account for the pain of migraine headache? The cartoon above [Figure 1]
shows how this can occur. The “skin” around the brain is highly
innervated with sensory nerve endings from the trigeminovascular system
(stemming from the trigeminal nerve (the 5th cranial nerve)) while the
brain itself has few sensory nerve endings.
(1) This means that when spreading depression occurs, in itself it is not painful.
(2) However, spreading depression causes a massive release of activating agents including potassium, nitric oxide, acid, and arachidonic acid that diffuse to local blood vessels in the skin of the brain (meninges) and activate the trigeminal nerve ending at the blood vessels there;
(3) This leads to activation of the bottom part of the trigeminal nucleus in the brain stem [13, 14];
(4) That ultimately can be perceived as pain. The distinction between “nociceptive” stimulus and pain perception is important. A stimulus like spreading depression produces a nociceptive response – that is a response capable of being registered as pain. This does not mean that a potentially painful stimulus (like migraine) always has a similar level of pain severity. Instead pain severity is a perception of pain. Here mood, situation or the circumstances at hand can markedly influence how bad a patient feels pain. For example, blood drawn from a needle stick to the arm generally is well-tolerated because one anticipates the stick and knows what it is. On the other hand, if a patient is in a completely darkened room and someone sneaks up on them and sticks them with the same needle, they are likely to be quite startled and consider the pain as much more severe. This is an important caveat to migraine control – namely a patient’s mood, lifestyle, can influence how they react to pain. Importantly, this also means that things like mood and lifestyle can be used to control pain.
(1) This means that when spreading depression occurs, in itself it is not painful.
(2) However, spreading depression causes a massive release of activating agents including potassium, nitric oxide, acid, and arachidonic acid that diffuse to local blood vessels in the skin of the brain (meninges) and activate the trigeminal nerve ending at the blood vessels there;
(3) This leads to activation of the bottom part of the trigeminal nucleus in the brain stem [13, 14];
(4) That ultimately can be perceived as pain. The distinction between “nociceptive” stimulus and pain perception is important. A stimulus like spreading depression produces a nociceptive response – that is a response capable of being registered as pain. This does not mean that a potentially painful stimulus (like migraine) always has a similar level of pain severity. Instead pain severity is a perception of pain. Here mood, situation or the circumstances at hand can markedly influence how bad a patient feels pain. For example, blood drawn from a needle stick to the arm generally is well-tolerated because one anticipates the stick and knows what it is. On the other hand, if a patient is in a completely darkened room and someone sneaks up on them and sticks them with the same needle, they are likely to be quite startled and consider the pain as much more severe. This is an important caveat to migraine control – namely a patient’s mood, lifestyle, can influence how they react to pain. Importantly, this also means that things like mood and lifestyle can be used to control pain.
HOW DO MIGRAINE TREATMENTS WORK?
Migraine
treatment begins with making the diagnosis. The diagnosis is made in
consultation with a physician. Ideally this doctor has expertise in
areas that include neurology, psychology/psychiatry, and pain management
and is kept up-to-date on headache care via research and patient care.
We’ve discussed the definition of migraine and these criteria are used to make the diagnosis. In addition, the physician performs a detailed neurological examination and reviews/orders all pertinent laboratory tests to help ensure the diagnosis by excluding other disease processes. Such tests cannot be specified beforehand but are used to rule out processes, when needed, other than migraine. Generally, no diagnostic test is needed to make the diagnosis of migraine. Furthermore, no diagnostic test is specific for migraine. From there, the doctor begins to formulate a treatment plan.
The first aspect of treatment is to consider lifestyle issues. Here caffeine use, sleep, meals, and exercise are especially important. Specific triggers of migraine (e.g., foods, alcohol, other beverages) are often a topic of the office visit. I generally make few restrictions on such triggers but remind patients that specific triggers like hot dogs, chocolate and cheeses can trigger migraine but often don’t do so in all patients. Thus, it may be best for each patient to discover what triggers migraine for them and then avoid these triggers as much as possible. For example, if wine triggers migraine, it generally will do so in minutes to at most a few hours after ingestion. Being a migraneur myself, my sense is that avoiding all foods that might trigger migraine would markedly deteriorate quality of life.
The other lifestyle issues noted above are more important. First, caffeine can be both a migraneur’s friend and enemy. Many migraine medicines include caffeine for an important reason. It can help stop migraine and amplifies the pain power of analgesics. However, drinking about two cups of coffee a day is enough to become addicted to caffeine. Caffeine withdrawal occurs about twelve hours after the last dose of caffeine and can trigger a migraine. This is often seen in patients who only drink caffeine in the morning and awaken with daily headaches. While other considerations for such headaches must be thought of at the doctor’s visit, a frequent culprit is the caffeine. If caffeine is spaced over the day (e.g., morning lunch, dinner), these headaches often disappear. The doctor and patient need to be sure that this use of caffeine does not prompt side-effects of insomnia, a racing heart, or nervousness. Of course if the latter occur, consideration should be given to removing caffeine completely.
Skipping meals is another notorious cause of migraine. It’s clear we’re all working more and too fast, so skipping meals sometimes becomes a part of our daily routine. However, for the migraneur, this can be especially harmful. Sitting down for a few minutes, relaxing and having a normal breakfast or dinner can reduce migraine. And the few minutes spent eating and briefly resting is far less than the time lost because of a migraine.
Sleep is another thing frequently given up by our work demands. Sleep deprivation can trigger migraine. In general, the doctor should help the patient discover how much sleep is likely to be enough to promote good health and feeling of being reasonably rested each morning. Typically, this is six to eight hours each night. If sleep is less than this or is interrupted more than once or twice in the night, consideration should be given to looking for (and treating as needed) a sleep disorder. Improved sleep, especially as we grow more mature, can go a long way to controlling headache. Strangely enough, sleeping too long can also trigger migraine. This type of migraine often appears on weekends as we sleep in. My sense is that these might stem, at least in part, from caffeine and food deprivation. Thus, my advice is usually to get up on the weekend at the same time as during the work week, have caffeine and breakfast and go back to sleep as a means to stop these headaches.
Next is exercise! This is often neglected by patients but often included by migraine specialists as an important adjunct to improving headache care. Let’s see why.
Migraine patients often show a history of family members with migraine. This has implied that migraine might be a genetic disorder. Indeed, recent research has tied three gene defects to migraine [15]. In each case these gene changes can increase the excitability of brain cells and so, make brain more susceptible to spreading depression, and so, migraine.
Much of my research is now directed to a theme recently articulated by Paul Silverman in a piece he wrote for The Scientist [4]. Dr. Silverman wrote that it is time to move past the notion of “genetic determinism.” Genetic determinism is a concept that suggests a gene defect necessarily determines whether a disease will appear. While this can be true in the extreme, it is most often not the case and certainly not the case with migraine. Instead Silverman argues that the environment of proteins made from the defective genes determines whether a disease becomes apparent. That is: Gene defects increase the likelihood a disease will appear, if the environment is right. This means those who carry a defective gene for migraine are more susceptible to get the headache from common triggers in the environment such as caffeine abstinence, skipping meals, lack of sleep, stress, etc.
As noted above, however, genetic propensity to migraine can be mitigated (or reversed) by environment. Environment for proteins is the milieu they are bathed in. Environment for patients includes how they live their lives and what they are exposed to. We’ve discussed several issues about this above but let’s focus on exercise. Numerous studies in animals and humans show that a wide range of neurological diseases can be lessened by increased social, intellectual and physical activity [16-18]. Many researchers, including those in my laboratory, are studying exactly how this comes about. While that is a lengthy topic for another time, the important take-home message is that casual exercise such as walking (especially in daylight) can reduce head pain. This only needs to be casual exercise and I suspect, is therapeutic because one’s mind tends to wonder (meditate?) during the exercise and so, the patient relaxes – while generating a brain more resilient to migraine!
We’ve discussed the definition of migraine and these criteria are used to make the diagnosis. In addition, the physician performs a detailed neurological examination and reviews/orders all pertinent laboratory tests to help ensure the diagnosis by excluding other disease processes. Such tests cannot be specified beforehand but are used to rule out processes, when needed, other than migraine. Generally, no diagnostic test is needed to make the diagnosis of migraine. Furthermore, no diagnostic test is specific for migraine. From there, the doctor begins to formulate a treatment plan.
The first aspect of treatment is to consider lifestyle issues. Here caffeine use, sleep, meals, and exercise are especially important. Specific triggers of migraine (e.g., foods, alcohol, other beverages) are often a topic of the office visit. I generally make few restrictions on such triggers but remind patients that specific triggers like hot dogs, chocolate and cheeses can trigger migraine but often don’t do so in all patients. Thus, it may be best for each patient to discover what triggers migraine for them and then avoid these triggers as much as possible. For example, if wine triggers migraine, it generally will do so in minutes to at most a few hours after ingestion. Being a migraneur myself, my sense is that avoiding all foods that might trigger migraine would markedly deteriorate quality of life.
The other lifestyle issues noted above are more important. First, caffeine can be both a migraneur’s friend and enemy. Many migraine medicines include caffeine for an important reason. It can help stop migraine and amplifies the pain power of analgesics. However, drinking about two cups of coffee a day is enough to become addicted to caffeine. Caffeine withdrawal occurs about twelve hours after the last dose of caffeine and can trigger a migraine. This is often seen in patients who only drink caffeine in the morning and awaken with daily headaches. While other considerations for such headaches must be thought of at the doctor’s visit, a frequent culprit is the caffeine. If caffeine is spaced over the day (e.g., morning lunch, dinner), these headaches often disappear. The doctor and patient need to be sure that this use of caffeine does not prompt side-effects of insomnia, a racing heart, or nervousness. Of course if the latter occur, consideration should be given to removing caffeine completely.
Skipping meals is another notorious cause of migraine. It’s clear we’re all working more and too fast, so skipping meals sometimes becomes a part of our daily routine. However, for the migraneur, this can be especially harmful. Sitting down for a few minutes, relaxing and having a normal breakfast or dinner can reduce migraine. And the few minutes spent eating and briefly resting is far less than the time lost because of a migraine.
Sleep is another thing frequently given up by our work demands. Sleep deprivation can trigger migraine. In general, the doctor should help the patient discover how much sleep is likely to be enough to promote good health and feeling of being reasonably rested each morning. Typically, this is six to eight hours each night. If sleep is less than this or is interrupted more than once or twice in the night, consideration should be given to looking for (and treating as needed) a sleep disorder. Improved sleep, especially as we grow more mature, can go a long way to controlling headache. Strangely enough, sleeping too long can also trigger migraine. This type of migraine often appears on weekends as we sleep in. My sense is that these might stem, at least in part, from caffeine and food deprivation. Thus, my advice is usually to get up on the weekend at the same time as during the work week, have caffeine and breakfast and go back to sleep as a means to stop these headaches.
Next is exercise! This is often neglected by patients but often included by migraine specialists as an important adjunct to improving headache care. Let’s see why.
Migraine patients often show a history of family members with migraine. This has implied that migraine might be a genetic disorder. Indeed, recent research has tied three gene defects to migraine [15]. In each case these gene changes can increase the excitability of brain cells and so, make brain more susceptible to spreading depression, and so, migraine.
Much of my research is now directed to a theme recently articulated by Paul Silverman in a piece he wrote for The Scientist [4]. Dr. Silverman wrote that it is time to move past the notion of “genetic determinism.” Genetic determinism is a concept that suggests a gene defect necessarily determines whether a disease will appear. While this can be true in the extreme, it is most often not the case and certainly not the case with migraine. Instead Silverman argues that the environment of proteins made from the defective genes determines whether a disease becomes apparent. That is: Gene defects increase the likelihood a disease will appear, if the environment is right. This means those who carry a defective gene for migraine are more susceptible to get the headache from common triggers in the environment such as caffeine abstinence, skipping meals, lack of sleep, stress, etc.
As noted above, however, genetic propensity to migraine can be mitigated (or reversed) by environment. Environment for proteins is the milieu they are bathed in. Environment for patients includes how they live their lives and what they are exposed to. We’ve discussed several issues about this above but let’s focus on exercise. Numerous studies in animals and humans show that a wide range of neurological diseases can be lessened by increased social, intellectual and physical activity [16-18]. Many researchers, including those in my laboratory, are studying exactly how this comes about. While that is a lengthy topic for another time, the important take-home message is that casual exercise such as walking (especially in daylight) can reduce head pain. This only needs to be casual exercise and I suspect, is therapeutic because one’s mind tends to wonder (meditate?) during the exercise and so, the patient relaxes – while generating a brain more resilient to migraine!
In fact, relaxation therapy,
biofeedback [19] and perhaps yoga are activities that can lessen
migraine because patients become less stressed. My suspicion is that
casual physical exercise acts in a similar way. More vigorous exercise
can worsen head pain, but otherwise may also be beneficial – especially
if it can include a meditative aspect. For example, walking or using a
treadmill can allow your mind to wonder, which can be nutritive. While
research in this area is just beginning, it appears that lifestyle
issues that help reduce migraine do so by altering gene expressions that
affect brain cell excitability.
When lifestyle adjustments alone are not enough, one needs to turn to pharmacological agents [20-22]. Here, important guidelines for headache management exist. First, if headaches occur infrequently (e.g., less than four times a month) an abortive agent – something that stops the progression of symptoms once started – can be used. Second, if the headaches occur more frequently or are prolonged, prophylactic or preventive therapy, usually daily, should be considered. Here, use of a headache diary that reports the number of headache days and headache intensity can be especially useful. Some doctors use a MIDAS (Migraine Disability Assessment) questionnaire for this purpose.
Acute migraine treatments are designed to stop the progression of headache symptoms once started. Acute treatments can be classified as specific (triptans) and non specific [TABLE 3]. Triptans are very effective in stopping acute migraine attacks. They do this by reducing activation of the trigemminal sensory nerve fibers that carry pain sensations from the meninges to the brain stem [23]. The triptans also trigger constriction of vascular smooth muscle in blood vessels. Less is known about how non specific treatments work [TABLE 3]. However, one important mechanism may be that non steroidal anti-inflammatory drugs (NSAIDS, which include ibuprofen and naproxen), which are very effective against migraine, can reduce inflammation; this in turn, can lessen pain at the meninges. Taken together, our knowledge of how acute treatments work centers on stopping the effects of spreading depression (the migraine) from developing painful stimuli. The initial trigger itself (spreading depression) has come and gone by the time a patient takes an abortive. Therefore, any affect of the abortive is on reducing what happens because of the spreading depression.
When lifestyle adjustments alone are not enough, one needs to turn to pharmacological agents [20-22]. Here, important guidelines for headache management exist. First, if headaches occur infrequently (e.g., less than four times a month) an abortive agent – something that stops the progression of symptoms once started – can be used. Second, if the headaches occur more frequently or are prolonged, prophylactic or preventive therapy, usually daily, should be considered. Here, use of a headache diary that reports the number of headache days and headache intensity can be especially useful. Some doctors use a MIDAS (Migraine Disability Assessment) questionnaire for this purpose.
Acute migraine treatments are designed to stop the progression of headache symptoms once started. Acute treatments can be classified as specific (triptans) and non specific [TABLE 3]. Triptans are very effective in stopping acute migraine attacks. They do this by reducing activation of the trigemminal sensory nerve fibers that carry pain sensations from the meninges to the brain stem [23]. The triptans also trigger constriction of vascular smooth muscle in blood vessels. Less is known about how non specific treatments work [TABLE 3]. However, one important mechanism may be that non steroidal anti-inflammatory drugs (NSAIDS, which include ibuprofen and naproxen), which are very effective against migraine, can reduce inflammation; this in turn, can lessen pain at the meninges. Taken together, our knowledge of how acute treatments work centers on stopping the effects of spreading depression (the migraine) from developing painful stimuli. The initial trigger itself (spreading depression) has come and gone by the time a patient takes an abortive. Therefore, any affect of the abortive is on reducing what happens because of the spreading depression.
It’s
different with prophylactic therapy. Here the basis for the efficacy
of agents such as anticonvulsants rest in the fact that these
medications reduce the tendency for spreading depression to occur [24]. The same may be true for calcium channel blockers [25].
As I discussed above, spreading depression begins when a sufficiently
large area of brain becomes over-excited. With time, prophylactic
medication [TABLE 4] can progressively reduce the tendency for
spreading depression (or migraine to occur). How beta-blockers or
tricyclic antidepressants produce a similar positive effect is less
known. However, this notion of a progressive or adaptive response of
brain to daily medications taken to stop migraine is worth discussing
further.
SUMMARY
The brain is a magnificently flexible organ designed to improve with use. It is not like a car, which deteriorates with use. Instead, it can be made more healthy and work better through increased use, which can include enhanced social, physical and intellectual activity. This actually builds a stronger brain; that is the brain adapts to become stronger and more resilient against migraine, as well as resistant against neurodegenerative diseases including Alzheimer’s disease, Parkinson’s disease, stroke and epilepsy. This concept can be an immensely empowering tool for patients, as well as a new direction for research efforts in migraine and neurodegenerative disease.REFERENCES
6. Lashley KS (1941) Patterns of cerebral integration indicated by scotomas of migraine. AMA Arch Neurol Psych 46:331-339.
7. Leão AAP (1944) Spreading depression of activity in the cerebral cortex. J Neurophysiol 7:359-390
7. Leão AAP (1944) Spreading depression of activity in the cerebral cortex. J Neurophysiol 7:359-390
TEXTS
While several texts on migraine are available, I found the publication by Drs. William B. Young and Stephen D. Silberstein particularly informative and complete:1. Young WS, Silberstein SD (2004) Migraine and Other Headaches. American Academy of Neurology Press: New York.
Another text is an excellent source for detailed information about headaches that is designed more for clinicians and researchers:
2. Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA (2006) The Headaches (3rd Edition). Lippincott Williams & Wilkins: Philadelphia.
WEB-BASED RESOURCES
Several outstanding web-based resources exist that are designed to help patients and families understand migraine. While not exhaustive, these sources include:
1. American Academy of Neurology (www.aan.com)
2. National Institute of Neurological Diseases and Stroke (www.ninds.nih.gov)
3. The Brain Matters (American Academy of Neurology; www.brainmatters.org)
4. National Headache Foundation (www.headaches.org)
5. American Council for Headache Education
1. American Academy of Neurology (www.aan.com)
2. National Institute of Neurological Diseases and Stroke (www.ninds.nih.gov)
3. The Brain Matters (American Academy of Neurology; www.brainmatters.org)
4. National Headache Foundation (www.headaches.org)
5. American Council for Headache Education
6. American Headache Society (http://www.americanheadachesociety.org/).
7. Society for Neuroscience (www.sfn.org)
8. In addition, I recently had the pleasure of co-authoring a migraine game entitled, “Head Defender” along with Drs. BS McEwen, MA Moskowitz, JR Saper, and SD Silberstein (http://www.cyberounds.com/games/hd) which may be of interest and fun to try. It is a continuing medical education game on migraine provided by Cyberounds®, a web-based continuing medical education tool whose Executive Editor is Harry A. Levy, M.D., M.P.H., Albert Einstein College of Medicine-Cyberounds (http://www.cyberounds.com).
ACKNOWLEDGEMENT
I am delighted to acknowledge
the outstanding assistance of those that created the videos used in
this “Knol” on migraine. My sense is that they dramatically enhance
understanding of the underlying mechanisms of migraine aura and migraine
pain. Mr. Dale Mertes and Roberto Marques of The University of Chicago
Networking Services and Information Technologies created videos 1, 2,
and 5. Ms. Jane Babiarz, an undergraduate student at The University of
Chicago working in my laboratory, edited video 3 and created, filmed and
edited video 4 illustrating the Belousov-Zhabotinsky reaction.
Our research into the mechanisms and consequences of spreading depression as well as the mechanisms of neurological preventive health has been funded by the National Institutes of Health via the National Institute of Neurological Disorders and Stroke for the past twenty-five years plus, the American Heart Association, Alzheimer’s Association, Brain Research Foundation, and the White Foundation.
The material with this Knol on migraine is for informational purposes only and it not intended as a substitute for a visit to a physician, which would include a professional medical interview, examination and medical advice, including diagnosis and formulation of a treatment plan.
Our research into the mechanisms and consequences of spreading depression as well as the mechanisms of neurological preventive health has been funded by the National Institutes of Health via the National Institute of Neurological Disorders and Stroke for the past twenty-five years plus, the American Heart Association, Alzheimer’s Association, Brain Research Foundation, and the White Foundation.
The material with this Knol on migraine is for informational purposes only and it not intended as a substitute for a visit to a physician, which would include a professional medical interview, examination and medical advice, including diagnosis and formulation of a treatment plan.